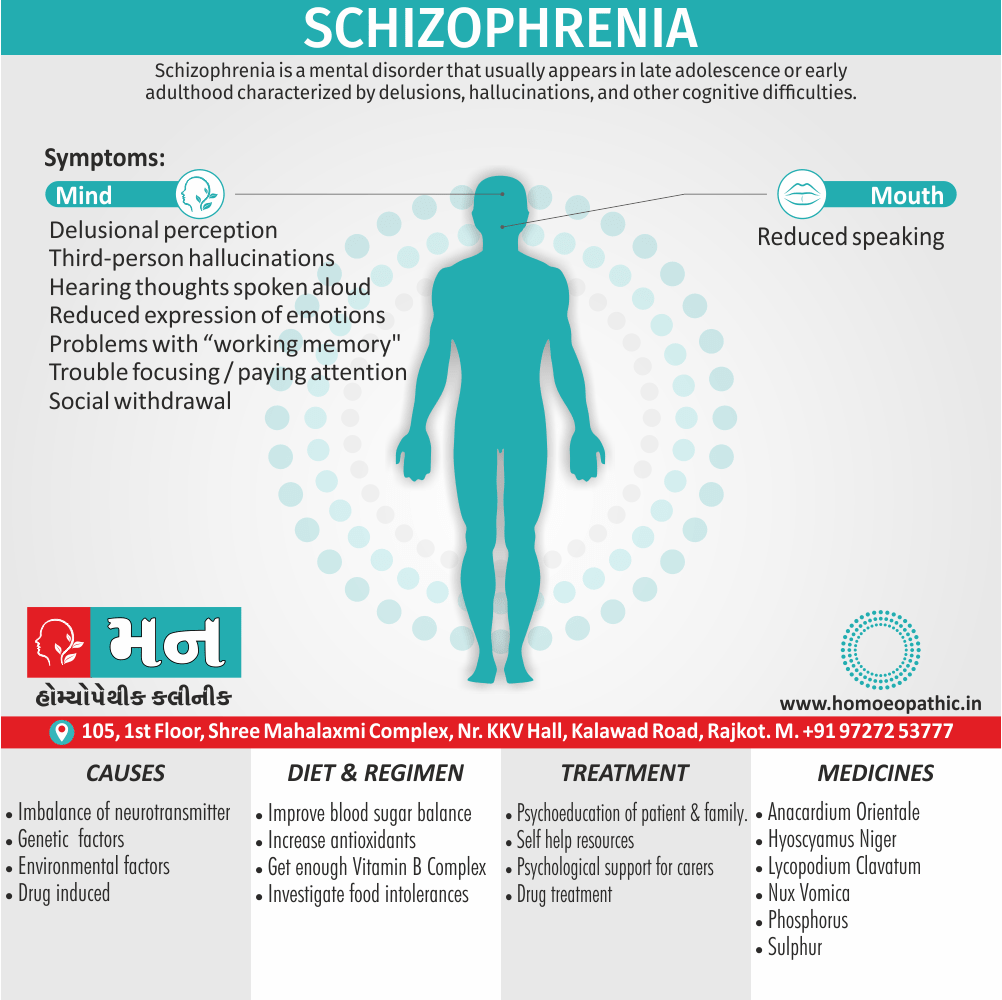
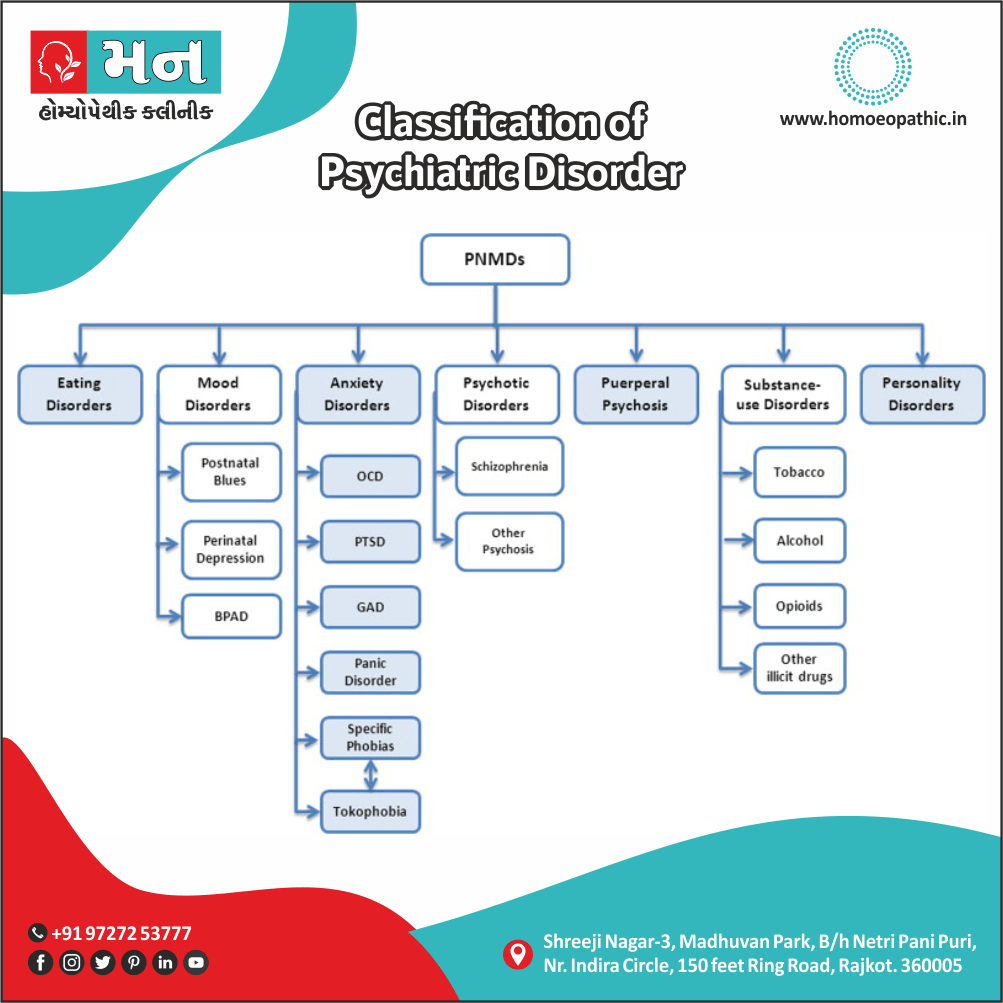
Schizophrenia:
Definition:
Schizophrenia and related disorders characterized by psychotic symptoms such as delusions and hallucinations.
There is a spectrum of severity. In schizophrenia, the patient suffers from psychotic symptoms and functional impairment. In delusional disorders, the patient experiences delusions, but there is no evidence of hallucinations or any of the other symptoms characteristic of schizophrenia.
Schizophrenia can be a particularly disabling illness because its course, although variable, is frequently chronic and relapsing.
The care of patients with schizophrenia places a considerable burden on all carers, from the patient’s family through to the health and social services,
General practitioners may have only a few patients with chronic schizophrenia on their lists but the severity of their problems also the needs of their families will make these patients important.
All in all, This Post aims to provide sufficient information for the reader to be able to recognize the basic symptoms of schizophrenia and related disorders and to be aware of the main homeopathic approaches to treatment. [2]
1. Paranoid schizophrenia:
Paranoid schizophrenia is characterised by delusions of persecution, reference, grandeur (or ‘grandiosity’), control, or infidelity (or ‘jealousy’).
The delusions are usually well systematised (i.e. thematically well connected with each other). The hallucinations usually have a persecutory or grandiose content.
The onset of paranoid schizophrenia is usually insidious, occurs later in life.
2. Hebephrenic (Disorganised) schizophrenia:
It is characterised by marked thought disorder, incoherence and severe loosening of associations. Delusions and hallucinations are fragmentary and changeable.
Emotional disturbances (inappropriate affect, blunted affect, or senseless giggling), mannerisms, ‘ mirror-gazing’ (for long periods of time), disinhibited behaviour, poor self-care and hygiene, markedly impaired social and occupational functioning, extreme social withdrawal and other oddities of behaviour.
3. Catatonic schizophrenia:
Catatonic schizophrenia (Cata: disturbed, tonic: tone) is characterised by a marked disturbance of motor behaviour, in addition to the general guidelines of schizophrenia described earlier.
It can present in three clinical forms: excited catatonia, stuporous catatonia, and catatonia alternating between excitement and stupor.
4. Residual schizophrenia:
It can present in three clinical forms: excited catatonia, stuporous catatonia, and catatonia alternating between excitement and stupor.
5. Undifferentiated schizophrenia:
This is a very common type of schizophrenia and is diagnosed either:
When features of no sub-type are fully present, or
When features of more than one sub-type are exhibited, and the general criteria for diagnosis of schizophrenia are met.
6. Simple schizophrenia:
Although called simple, it is one of the sub types which is the most difficult to diagnose.
It is characterised by an early onset (early 2nd decade), very insidious and progressive course, presence of characteristic ‘negative symptoms’ of residual schizophrenia (such as marked social withdrawal, shallow emotional response, with loss of initiative and drive), vague hypochondriacal features, a drift down the social ladder, and living shabbily and wandering aimlessly.
7. Post-schizophrenic depression:
Some schizophrenic patients develop depressive features within 12 months of an acute episode of schizophrenia.
The depressive features develop in the presence of residual or active features of schizophrenia and are associated with an increased risk of suicide.
8. Others:
- Pseudoneurotic Schizophrenia
- Schizophreniform Disorder
- Oneiroid Schizophrenia
- Van Gogh Syndrome
- Late Paraphrenia
- Graft Schizophrenia
- Type I and Type II Schizophrenia. [1]
Symptoms of schizophrenia usually start between ages 16 and 30. In rare cases, children have schizophrenia too.
The symptoms of schizophrenia fall into three categories: positive, negative, and cognitive.
Positive symptoms:
“Positive” symptoms are psychotic behaviors not generally seen in healthy people. People with positive symptoms may “lose touch” with some aspects of reality.
Symptoms include i.e.:
- Hallucinations.
- Delusions.
- Thought disorders (unusual or dysfunctional ways of thinking).
- Movement disorders (agitated body movements).
Negative symptoms:
“Negative” symptoms are associated with disruptions to normal emotions and behaviors.
Symptoms include i.e.:
- “Flat affect” (reduced expression of emotions via facial expression or voice tone).
- Reduced feelings of pleasure in everyday life.
- Difficulty beginning and sustaining activities.
- Reduced speaking.
Cognitive symptoms:
For some patients, the cognitive symptoms of schizophrenia are subtle, but for others, they are more severe and patients may notice changes in their memory or other aspects of thinking.
Symptoms include i.e.:
- Poor “executive functioning” (the ability to understand information and use it to make decisions).
- Trouble focusing or paying attention.
- Problems with “working memory” (the ability to use information immediately after learning it).
Schneider’s ‘first-rank’ symptoms of schizophrenia:
- Hearing thoughts spoken aloud.
- Third-person’ hallucinations.
- Hallucinations in the form of a commentary.
- Somatic hallucinations.
- Thought either withdrawal or insertion.
- Thought broadcasting.
- Delusional perception.
- Either Feelings or actions experienced as made or influenced by external agents. [2]
There is strong evidence for genetic causes, and good reason to believe that stressful life events may provoke the disorder.
1. Genetic factors:
There is strong evidence for the heritability of schizophrenia from three sources.
- Family studies: Schizophrenia is more common in the relatives of schizophrenic patients that in the general population (where the lifetime risk is approximately 1 per cent). Additionally, The risk is 10–15 per cent in the siblings of schizophrenics.
- Twin studies: It indicate that a major part of this is due to genetic rather than to environmental factors. Among monozygotic twins, the concordance rate (the frequency of schizophrenia in the sibling of the affected twin) is consistently higher than among dizygotic twins.
- Adoption studies: Among children who have been separated from a schizophrenic parent at birth also brought up by non schizophrenic adoptive parents, the likelihood of developing schizophrenia is no less than that among children brought up by their own schizophrenic parent.
- Specific genes: DISC1, Dysbindin, Neuregulin-1, MHC locus, ZNF804A and G72.
2. Environmental factors:
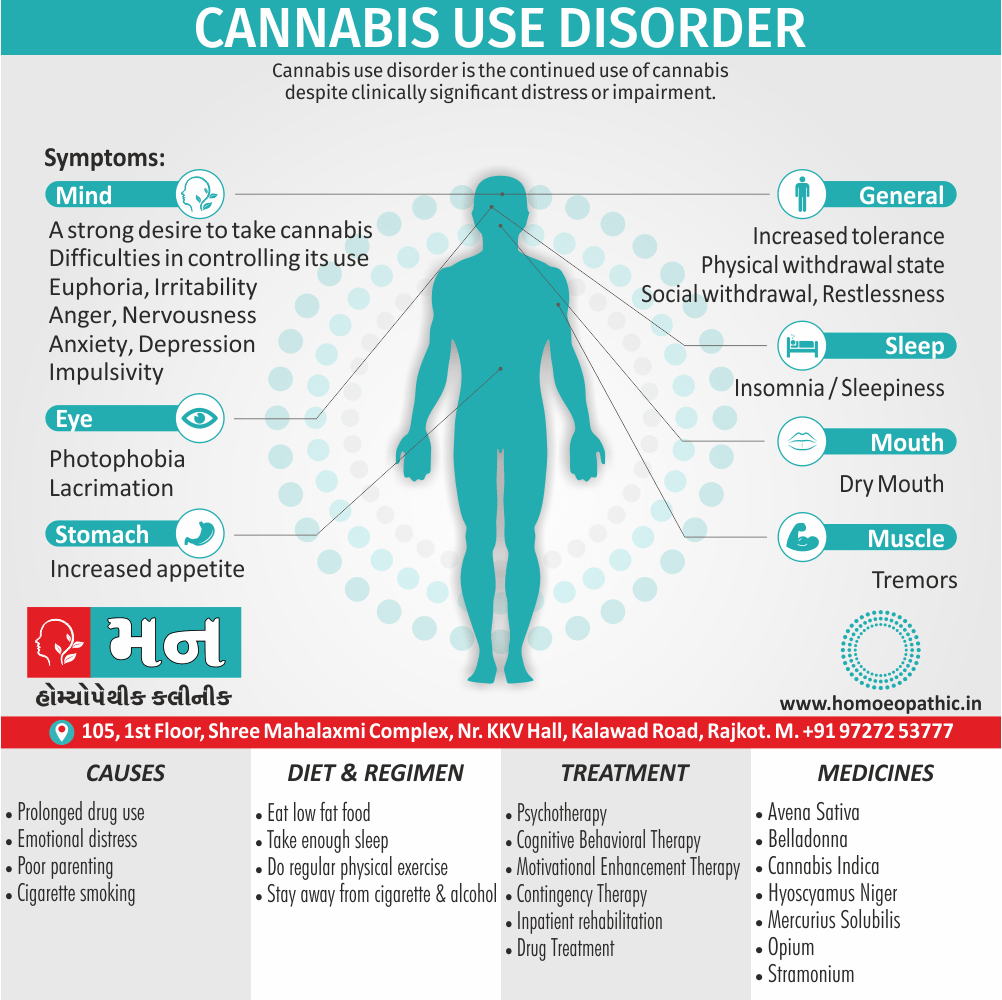
- Predisposing factors: Abnormalities of pregnancy and fetal development are risk factors, although the size of the association is small. Although it may involve fetal hypoxia. There is also an association with low social class, social deprivation increases exposure to several risk factors. Besides this, There is some evidence that heavy cannabis consumption is associated with the development of schizophrenia.
- Precipitating factors: It include stressful life events occurring shortly before the onset of the disorder.
- Maintaining factors: They include strongly expressed feelings, especially in the form of critical comments, among family members (‘high emotional expression’). High expressed emotion may lead to increased relapse rates and can be modified by family therapy. [2]
The diagnosis of schizophrenia is based entirely on the clinical presentation (history and examination).
The currently most widely used diagnostic criteria are those in the International Classification of Diseases (ICD10) and the Diagnostic and Statistical Manual of the American Psychiatric Association (DSM-IV).
Appearance and behaviour:
Preoccupied, withdrawn, Restless, noisy, inconsistent.
Mood:
- Mood change
- Blunting, Incongruity.
Disorders of thinking:
- Vagueness.
- Formal thought disorder
- Disorders of the stream of thought.
Hallucinations:
- Auditory
- Visual
- Tactile, olfactory, gustatory.
Delusions:
- Primary
- Secondary (especially persecutory)
Orientation: Normal
Attention: Impaired
Memory: Normal
Insight: Impaired.
Schneider’s ‘first rank’ symptoms are also useful.
Impaired social and occupational functioning.
A minimum duration (6 months in DSM-IV but, unfortunately, a different period—1 month—in ICD-10).
The exclusion of (i) organic mental disorder, (ii) major depression, (iii) mania, or (iv) the prolongation of autistic disorder. [2]
1. Hospital management of an acute episode of schizophrenia:
- Antipsychotic medication.
- Appropriate activities.
- Counselling for patient and family.
- Good response and good prognosis: Continue medication for 6 months, gradual return to work and social activities. And regular review and counselling.
- Incomplete response and/or poor prognosis: Long-term medication (consider depot), counselling and support for family (reduce ‘expressed emotion) and assess needs for sheltered work or housing. [2]
2. Antipsychotic drug therapy:
Most anti psychotic drugs have an immediate sedative effect, followed by an effect on psychotic symptoms (especially hallucinations and delusions), which may take up to 3 weeks to develop fully.
Risperidone (Risperdal) i.e.-
less sedating than other atypical antipsychotics. Weight gain and diabetes are possible side effects, but are less likely to happen, compared with Clozapine or Olanzapine.
Olanzapine (Zyprexa) i.e. –
may also improve negative symptoms. However, the risks of serious weight gain and the development of diabetes are significant.
Quetiapine (Seroquel) i.e.-
risk of weight gain and diabetes, however, the risk is lower than Clozapine or Olanzapine.
Ziprasidone (Geodon) i.e.-
the risk of weight gain and diabetes is lower than other atypical antipsychotics. However, it might contribute to cardiac arrhythmia.
Clozapine (Clozaril) i.e.-
effective for patients who have been resistant to treatment. It is known to lower suicidal behaviors in patients with schizophrenia. The risk of weight gain and diabetes is significant.
Haloperidol i.e.-
an antipsychotic used to treat schizophrenia. It has a long-lasting effect (weeks).
The primary schizophrenia treatment is medication. Sadly, compliance (following the medication regimen) is a major problem. The patient must continue taking medication even when symptoms are gone. Otherwise they will come back.
3. Electroconvulsive Therapy (ECT):
Schizophrenia is not a primary indication for ECT. The indications for ECT in schizophrenia include:
1. Catatonic stupor.
2. Uncontrolled catatonic excitement.
3. Acute exacerbation not controlled with drugs.
4. Severe side-effect with drugs, in presence of untreated schizophrenia.
Usually 8-12 ECTs are needed (although up to 18 have been given in poor responders), administered two or three times a week.
4. Psychosurgery:
Psychosurgery is not routinely indicated in the treatment of schizophrenia. When used, the treatment of choice is limbic leucotomy (a small subcaudate lesion with a cingulate lesion) in some cases with severe and very prominent depression, anxiety or obsessional symptoms.
5. Psycho social Treatment:
Psycho social treatment is an extremely important component of comprehensive management of schizophrenia.
It can be divided in following steps:
Psycho education: of the patient and especially the family/carers (with patient’s consent) regarding the nature of illness, and its course and treatment.
Group psychotherapy: It is particularly aimed at teaching problem solving and communication skills.
Family therapy: Apart from psycho education, family members are also provided social skills training to enhance communication and help decrease intrafamilial ‘tensions’.
Milieu therapy (or therapeutic community): It includes treatment in a living, learning or working environment ranging from in patient psychiatric unit to day-care hospitals and half-way homes.
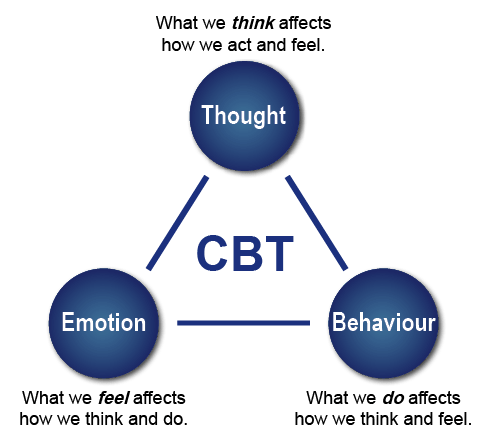
Individual psychotherapy: It is usually supportive in nature. Several centers (and guidelines) recommend the use of cognitive behaviour therapy (in other words; CBT) in the treatment of schizophrenia.
Psychosocial rehabilitation: It is used, usually along with milieu therapy. Furthermore, This includes activity therapy, to develop the work habit, training in a new vocation or retraining in a previous skill, vocational guidance, independent job placement, sheltered employment or self-employment, and occupational therapy.
However, anti psychotic drug treatment in the acute stages, as well as for maintenance treatment, is the mainstay of management of schizophrenia. [1]
1.Stramonium:
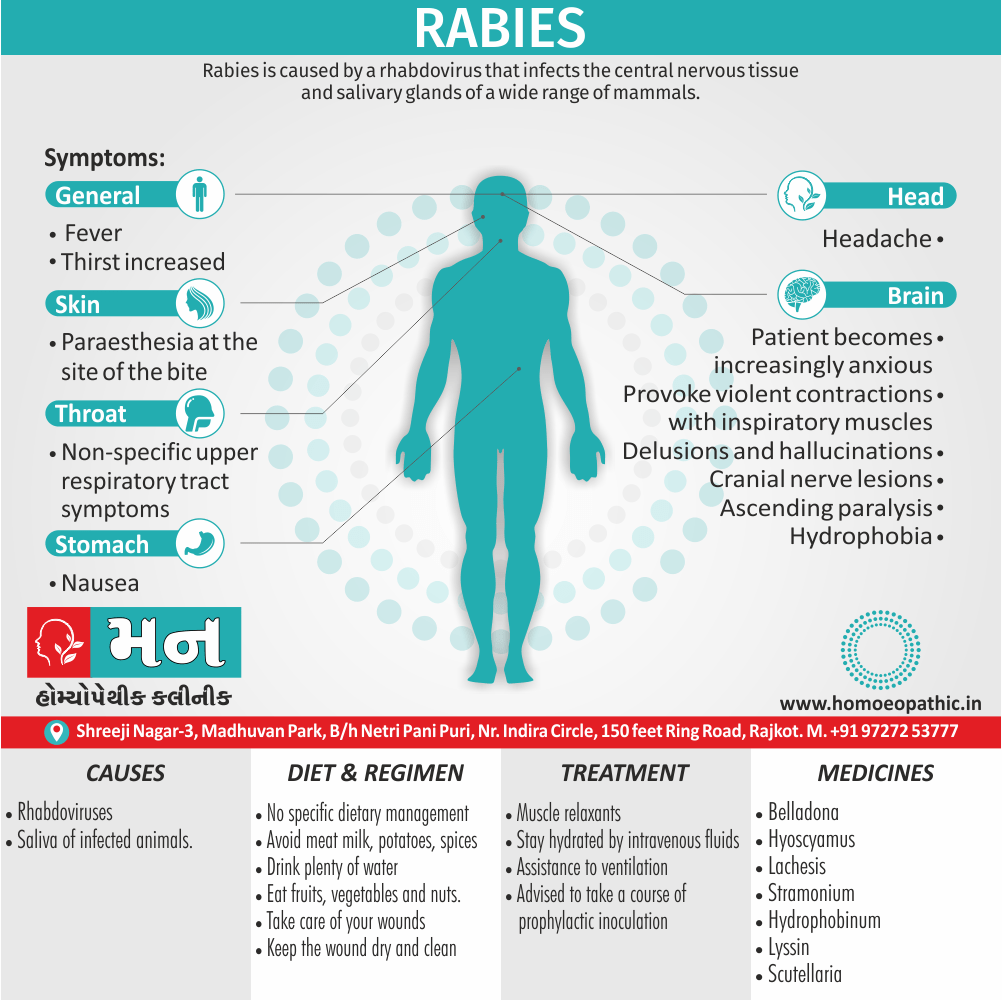
High energy and intensity are striking in this remedy. Violence or fear of violence is a keynote. Night is a good time to look for Stramonium symptoms because they are afraid of the dark, they are worse at night and may need all the lights on in the room; a hall light or night light may not be sufficient. Night Terrors-shrieking in sleep, tossing and turning, sitting up and not knowing anyone, terrified, and not remembering the event the next morning, especially in children, is characteristic. A high fever, a suppressed fever, a stroke, meningitis, a recent fright or a fright they’ve never got over, sunstroke, a dog bite, a head injury, rabies, and alcoholism, are all possible causes.
Other Stramonium symptoms include-ceaseless talking, fear of tunnels, desire to escape, eyes staring wide, eyes half open during sleep. Face expression of terror-believes he is possessed by the devil or has other issues with the devil or devils. There may be an absence of pain where pain would be normal. Raving mania, super-human strength, dilated pupils, red face, violent rages, manic-depression, biting, striking, strangling.
Other symptoms
Fear of water, including the sight of running water, the sound of water, getting the head wet in the shower or the swimming pool, fear of shining objects, reflecting objects, glittering objects, mirrors, fear of animals, dogs, disease, ghosts, suffocation, claustrophobia, death, anything like death, such as the colour black or cemeteries, etc. Conversely, they may dress all in black or seek out cemeteries and the like. Fear of being alone, better with company, especially at night. Stammering-makes explosive efforts to get the first syllable out grimacing, twitches. Hallucinations-sees animals coming at him, sees ghosts, talks to spirits, hears voices.
(All the insanity remedies seem to have religious affections-praying, talking to God, believing he is some great religious figure, etc. So, we can’t rely on this feature to differentiate among them.)
Lachesis:
Intense people, egotistical, arrogant. This remedy is especially associated with an excessive use of alcohol. Locquacious, jumping from one subject to another. The patient talks a lot and talks loud! Lachesis knows how to strike at the weak points of others and devastate them; sarcastic wit. Think of the sharp fangs of the snake and how they will suddenly strike when least expected. Jealous and envious, very possessive and suspicious that the partner is cheating.
The Lachesis husband will listen in on the wife’s phone conversations, go through her personal papers, have her followed, watch her carefully when she’s with other men, and finally will make an outrageous statement, like, “I know you’re seeing Melvin Flurg !” The wife will say, “I do not even like Melvin Flurg !” But eventually it becomes a self- fulfilling prophesy because the wife gets fed up and leaves, but not without a restraining order ! Lachesis is suspicious in general of everyone’s intentions, which can escalate into paranoia. Suspicious of you, the homoeopath, the remedy, and probably will refuse to take it, and will suspect you of trying to poison him.
Other symptoms
As Lachesis is venom, look for them to have a big issue with poisoning. Snake venom causes the victim to haemorrhage, so, think of bleeding problems in Lach. Patients, such as nosebleeds or history of nosebleeds. In fact, think of disturbances of the blood-the vascular system, the cardio vascular system, high blood pressure, heart disease, hot flushes of menopause. Discharges ameliorate–that means that the headache will improve with a nasal discharge, or PMS will get better when the menstrual flow begins. Any discharge may make the person feel better-you can even think of talking as a discharge, a flow of words, which is why they will talk and talk and talk; conversely, stopping or suppressing normal discharges will aggravate a Lachesis person.
Think of how a snake can be completely controlled by being grabbed around the throat; therefore, Lachesis people cannot bear tight collars or tight clothes in general. Find out what the person wears when he can wear anything he wants. Similarly, the Lachesis person cannot tolerate any “tight” or “restricting” situation! For example, working under authority, having to adhere to a schedule, having to answer to someone they may be angry, aggressive, sarcastic, hate-filled and vengeful. Sleep is not their friend ! Sleep is a very bad time for Lachesis ! They may have insomnia, or they may wake worse than they were before they went to sleep.
Waking with a feeling of suffocation is a common complaint in Lachesis. Left-sided complaints, or complaints that start on the left and move to the right. Lachesis people are hot and better from cool/cold open air also cold drinks. Fear of heart attacks, suffocating, or snakes, or they may really like snakes and think they’re interesting. Lastly, They may have a fear that they’re being followed, delusion, someone is behind them.
3. Hyoscyamus:
Loquacious, suspicious and jealous. The etiology for this state may dis- appointed love or rejection. Mania, rage, aggression, increased strength, delusion he will poison, delusion he is pursued by the police, delusion he sees ghosts and spirits, fear of poison, dogs, animals, water. Ability or desire to kill. Mania and rage, desire to break things. Attempts to escape.
What Hyoscyamus well known for is-lewdness, loud laughter, nudity, undressing in public, shamelessness, cursing, wild talking, dancing, silly and foolish behaviour, jesting, making strange gestures, restless fingers, “Picking”-picking anything, like imaginary things in the air.. picking the bedspread, the clothing, and so on. Fear of being alone, desires company. Restlessness. Sleepless from mental agitation, nightmares. Suspicious and fear of being poisoned. Talks rapidly, changes subjects of- ten, laughs immoderately; rolls on the ground, dances, gesticulates, and in general behaves wildly and shamelessly. In the Repertory, “Mind: insanity, chaotic person, behaves like a”Hyoscyamus is the only “3” in this rubric (which means the only remedy highly indicated.for this behaviour).
4. Anacardium:
The idea in this remedy is a divided self, or the idea of being separate; separate from the family or group, separate from society-doesn’t fit in; and in general, two selves divided. He might described as a devil by some and an angel by others. They might believe that he possessed by the devil. They may say that he hears voices and the voices tell him what to do. He may sense the presence of “others” or another, where no one is there.
The remedy itself in its physical form is a nut (no pun intended) that is very sweet on the inside and hard and caustic on the outside, which very aptly explains this remedy-hard, as in no feeling for the suffering of others or the suffering that he may cause. These are the people who can very cruel to animals. The Anacardium person may someone who pressured by domineering parents to become something the parents could . be proud of. Unable to achieve this, he has both anger and low self esteem. His most often repeated phrase might be “I hate … !” ( “I hate my life, I hate school, and I hate everyone!”).
There is a lot of cursing, shouting, acting in cruel and malicious ways, especially if he’s a child or adolescent who’s been beaten and abused in childhood, which is frequently the etiology for this remedy. Some important characteristic symptoms of this remedy are indecision. Consistent with his divided self, he finds deciding between one thing and another next to impossible and exasperating, poor memory.
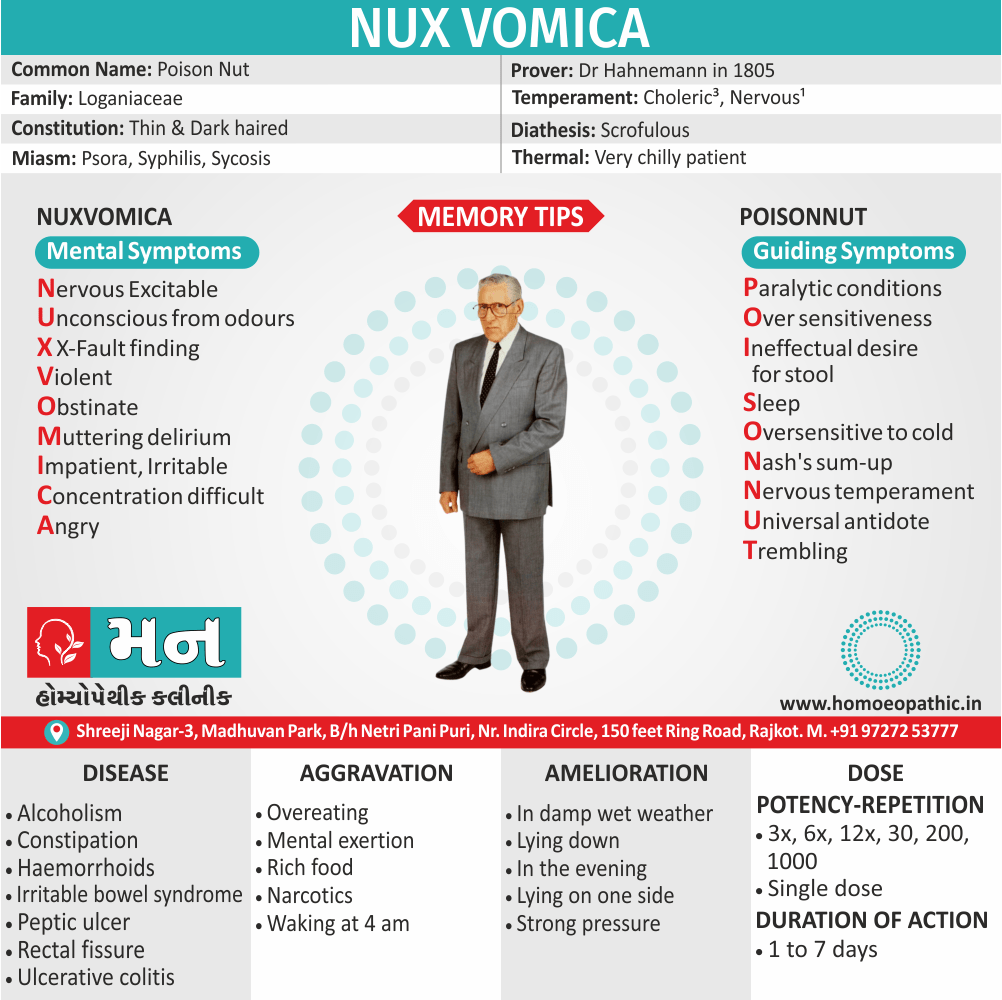
5. Nux vomica:
The key ideas for this remedy arc over-sensitive, over-achieving and need for stimulation. When you think about it, everything that’s wrong with Nux Vomica springs from here. Let’s start with over-achieving. This is not your remedy for timidity and low self-esteem! Nux Vomica sees what it wants, has a goal, and goes after it; nothing can stop Nux Vomica ! These people are focused! Just try and stop them! These are football players who plow their way ·into the end zone; they do not care if they get hurt or who’s in their way ! They want power, they do riot shrink from confrontation, and in fact they welcome it-just itching for a fight! Bring on the competition! This is because of their need for stimulation (which may explain their desire for spicy food-in fact, their lives are anything but bland!)
They crave stimulation, challenges. Their idea of relaxing is to take on more work! (“occupation ameliorates”) But this constant need for stimulation can be problematic. The Nux Vomica “family man” simply can’t.be content in a tranquil, peaceful home. Such bland surroundings would irritate him immensely. So Mr. Nux Vomica finds fault with everything and everyone in his home: Dinner wasn’t served on time! Someone’s sitting in his chair! And if Mr. Nux Vomica has a drinking problem (and he probably does) look out! They have a fiery temper-so angry they could kill! Explosions! outbursts!
Other symptoms
This is the house where the wife and the kids are walking on eggshells be- cause they do not know what’s going to happen next! ‘And after he’s got everyone in the house crying, screaming and yelling, he’ll say, “Shhh ! I need to be quiet!” Yes, what nerve! ( oversensitivity, easily irritated.) Because of all of Nux Vomica’s bad habits-his overwork, lack of sleep-the famous Nux vomica insomnia-use of drugs and coffee and alcohol (stimulants), his nerves are frayed! He can’t tolerate interruptions, he can’t tolerate noise; in fact, in order to work, he must have complete quiet.
To go to sleep, Mr Nux Vomica requires complete quiet! Odours also bother him. In fact, any disharmony in the environment at all is intolerable. He may say things like, “My house is a constant irritation to me!” Everything he does is done perfectly and systematically with attention to detail and efficiency, and do not you try to help because you won’t know how! Furthermore, He can’t delegate authority because everyone is so stupid, so incompetent! He won’t even let the family order in a restaurant for themselves. If the wife orders fish, he’ll say, “You do not want the fish. The fish is no good here. I’ll just handle this. Waiter, my wife will have the roast beef.”.
Frequently Asked Questions
What is Schizophrenia?
Schizophrenia and related disorders characterized by psychotic symptoms such as delusions and hallucinations.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Schizophrenia?
- Stramonium
- Lachesis
- Hyoscyamus
- Anacardium
- Nux vomica
What are the main types of Schizophrenia?
- Paranoid schizophrenia
- Hebephrenic schizophrenia
- Catatonic schizophrenia
- Residual schizophrenia
- Undifferentiated schizophrenia
- Simple schizophrenia
- Post-schizophrenic depression
What are 5 causes of Schizophrenia?
- Genetic factors
- Abnormalities of pregnancy and fetal development
- low social class, social deprivation
- stressful life events
- strongly expressed feelings
Give the first 5 symptoms of Schizophrenia?
- Hallucinations.
- Delusions.
- Thought disorders
- Movement disorders
- Negative symptoms
- A Short Textbook of PSYCHIATRY 7th edition by Niraj Ahuja / ch 5.
- Psychiatry, Fourth Edition – Oxford Medical Publications -SRG-by John Geddes, Jonathan Price, Rebecca McKnight / ch 22.
- https://www.medicalnewstoday.com/articles/36942.php
- Homeopathy in treatment of Psychological Disorders by Shilpa Harwani / ch 13.