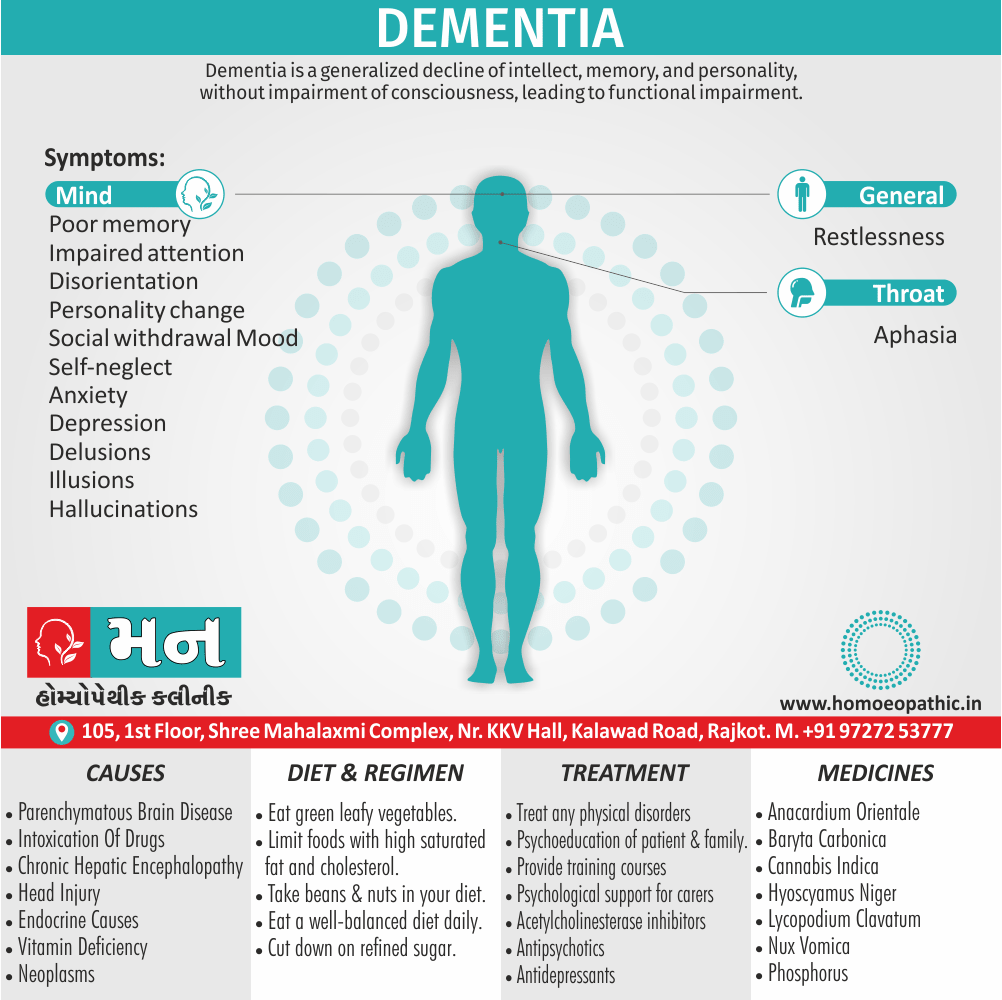
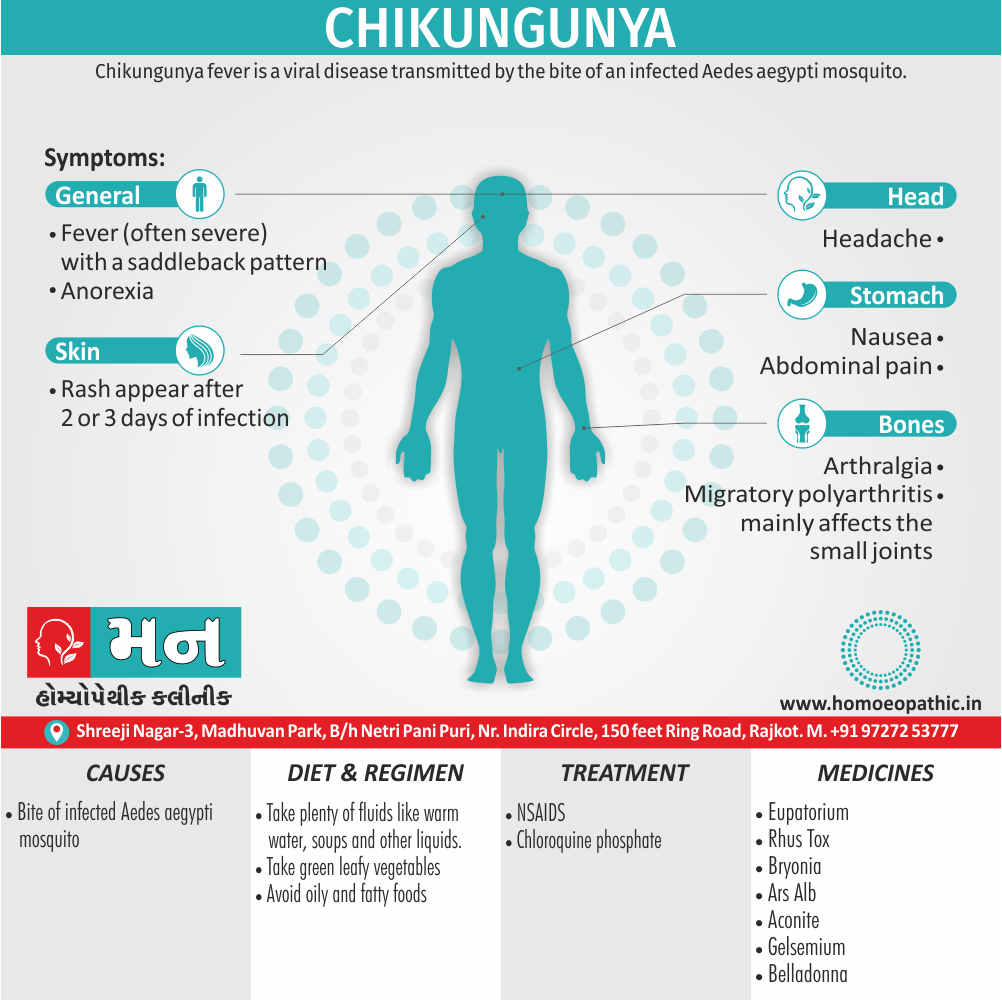
It is a clinical syndrome, rather than a diagnosis in itself, which may cause by a variety of pathologies. Dementia is an acquired disorder, as distinct from learning disability in which impairments are present from birth, although the onset may be at any age.
In either middle-aged or older person any social lapse that is out of character should always suggest dementia. [1]
Onset: Insidious
Course: Protracted, although may be reversible in some cases. [2]
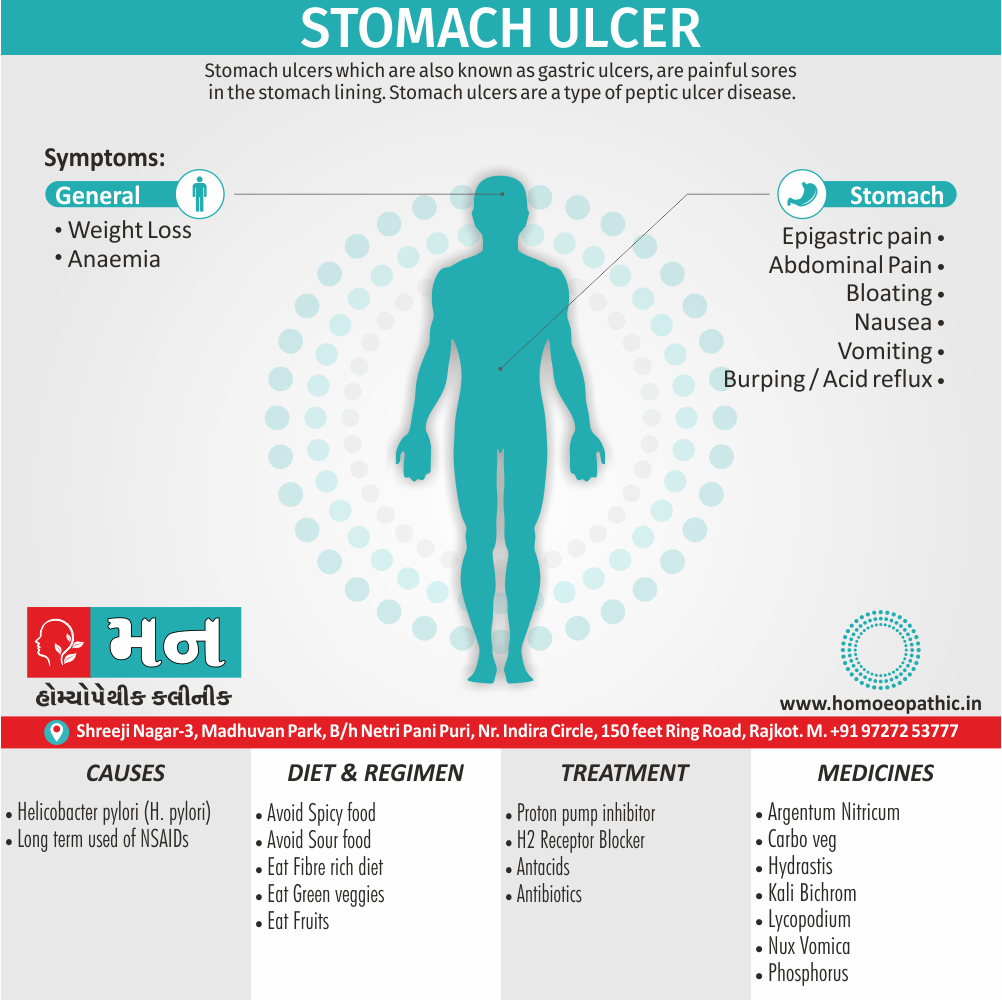
Irreversible causes:
Parenchymatous brain disease i.e.:
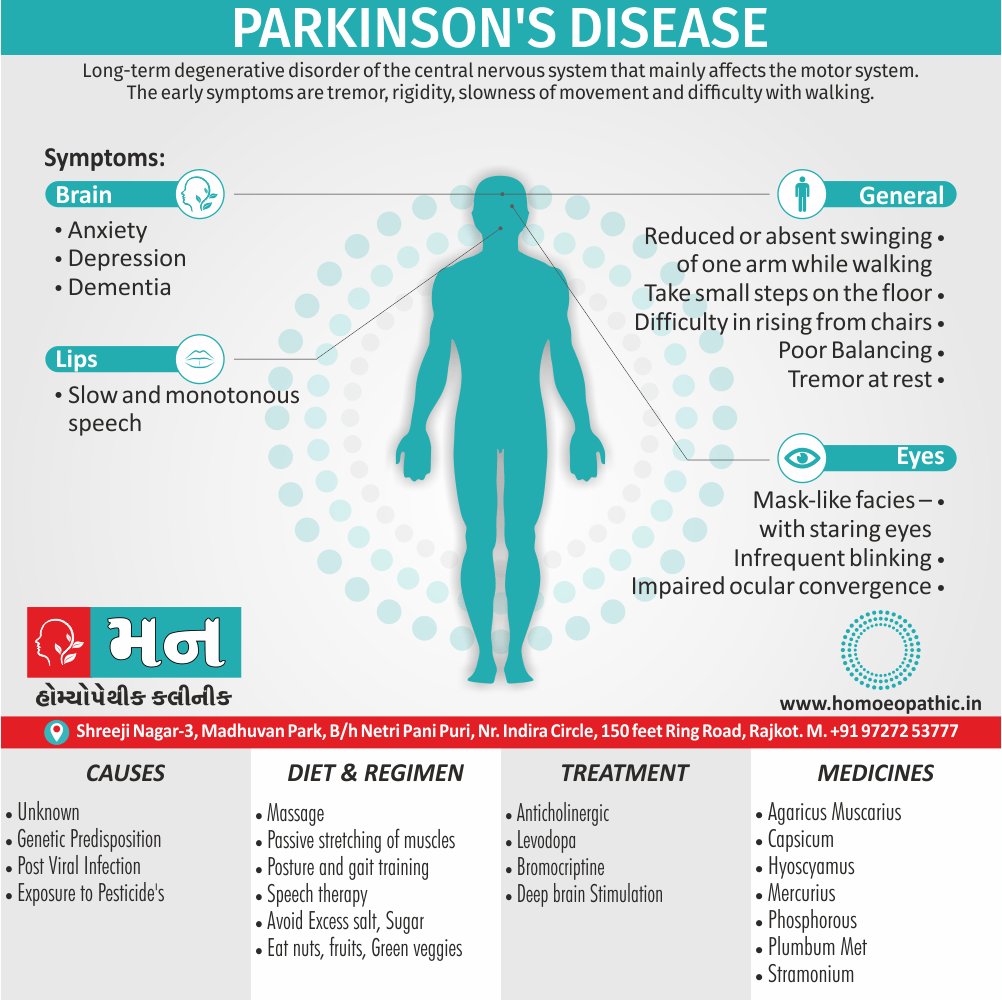
Alzheimer’s disease, Pick’s disease, Parkinson’s disease, Huntington’s chorea, Lewy body dementia, Steel Richardson syndrome ( in other words, Progressive Supranuclear Palsy).
Vascular dementia i.e.:
Multi-infarct dementia, subcortical vascular dementia ( in other word, Binswanger’s disease).
Toxic dementias i.e.:
Bromide intoxication, drugs, heavy metals, alcohol, carbon monoxide, analgesics, anticonvulsants, benzodiazepines, also psychotropic drugs.
Metabolic dementias i.e.:
Chronic hepatic or uraemic encephalopathy, dialysis dementia, Wilson’s disease.
Traumatic dementias i.e.:
Chronic subdural haematoma, head injury.
Potentially reversible causes:
Endocrine causes i.e.:
Thyroid, parathyroid, pituitary, also adrenal dysfunction.
Deficiency Dementias i.e.:
Pernicious anaemia, pellagra, folic acid deficiency, also thiamine deficiency.
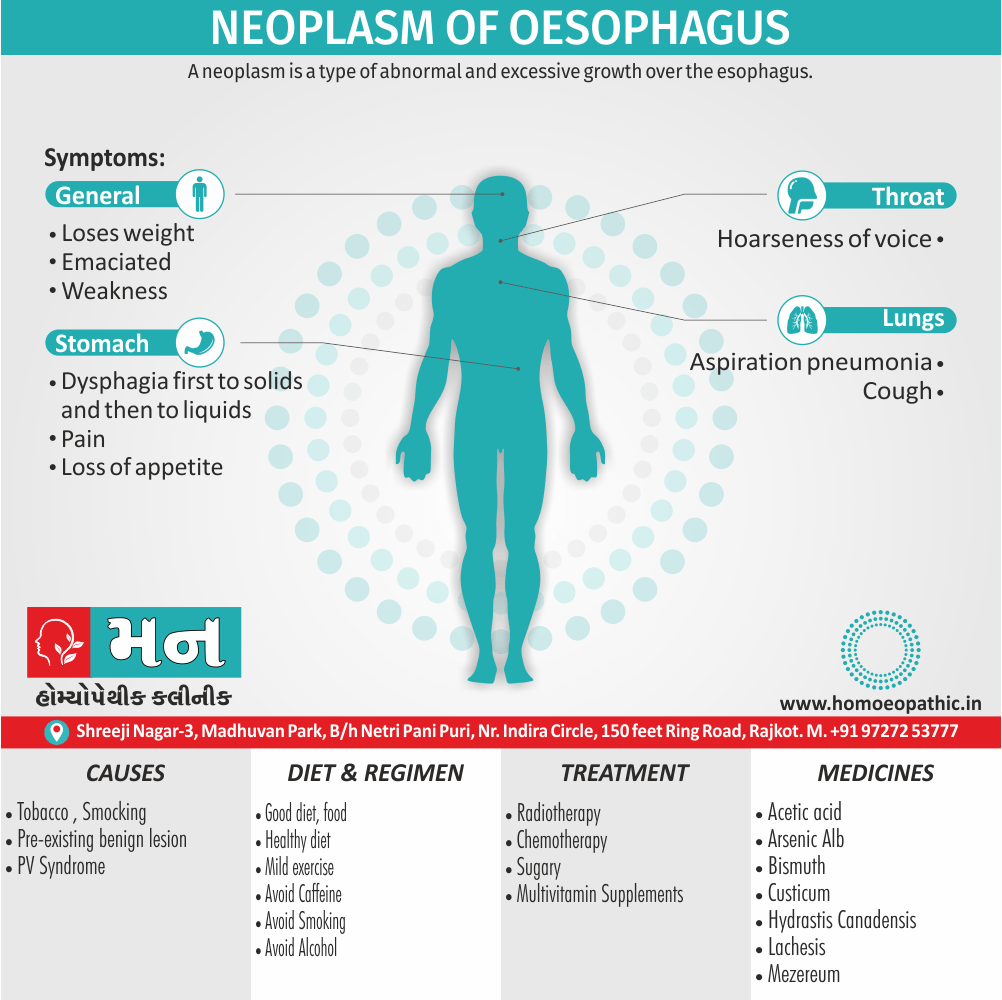
Neoplastic dementias i.e.:
Neoplasms and other intracranial space-occupying lesions.
Hydrocephalic dementia i.e.:
Normal pressure hydrocephalus. [2]
Risk factor of Dementia
Age. – The risk of Alzheimer’s disease, vascular dementia, and several other dementias goes up significantly with advancing age.
Genetics/family history- Researchers have discovered a number of genes that increase the risk of developing Alzheimer’s disease. Although people with a family history of Alzheimer’s disease are generally considered to be at a heightened risk of developing the disease themselves, many people who have relatives with Alzheimer’s disease never develop the disease, and many without a family history of the disease do get it.
Smoking and alcohol use- Several recent studies have found that smoking significantly increases the risk of mental decline and dementia. People who smoke have a higher risk of atherosclerosis and other types of vascular disease, which may be the underlying causes for the increased dementia risk.
Atherosclerosis.- Atherosclerosis is the buildup of plaque – deposits of fatty substances, cholesterol, and other matter – in the inner lining of an artery.
Atherosclerosis is a significant risk factor for vascular dementia, because it interferes with the delivery of blood to the brain and can lead to stroke. Studies have also found a possible link between atherosclerosis and Alzheimer’s disease.
Cholesterol- High levels of low-density lipoprotein (LDL), the so-called "bad" form of cholesterol, appear to significantly increase a person’s risk of developing vascular dementia. Some research has also linked high cholesterol to an increased risk of Alzheimer’s disease.
Plasma homocysteine- Research has shown that a higher-than-average blood level of homocysteine, a type of amino acid, is a strong risk factor for the development of Alzheimer’s disease and vascular dementia.
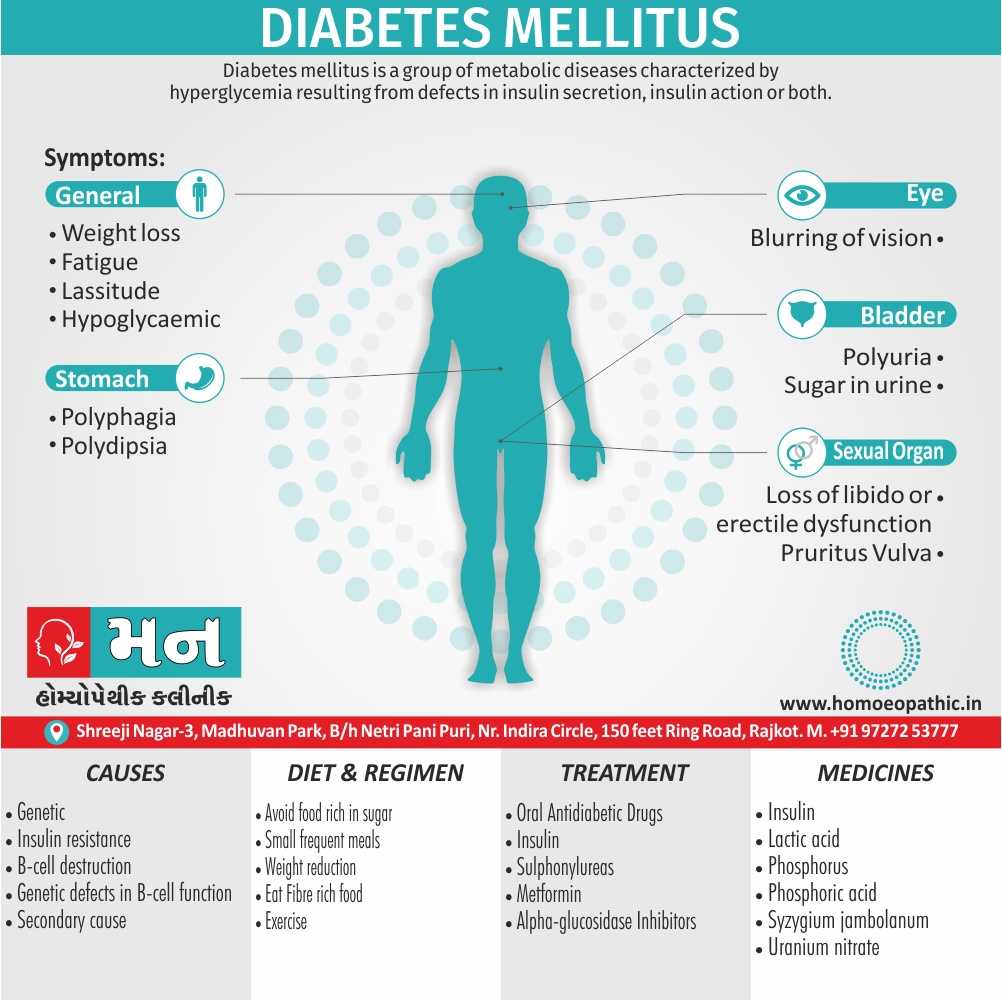
Diabetes- Diabetes is a risk factor for both Alzheimer’s disease and vascular dementia. It is also a known risk factor for atherosclerosis and stroke, both of which contribute to vascular dementia.
Mild cognitive impairment- While not all people with mild cognitive impairment develop dementia, people with this condition do have a significantly increased risk of dementia compared to the rest of the population.(4)
Pathophysiology of Dementia
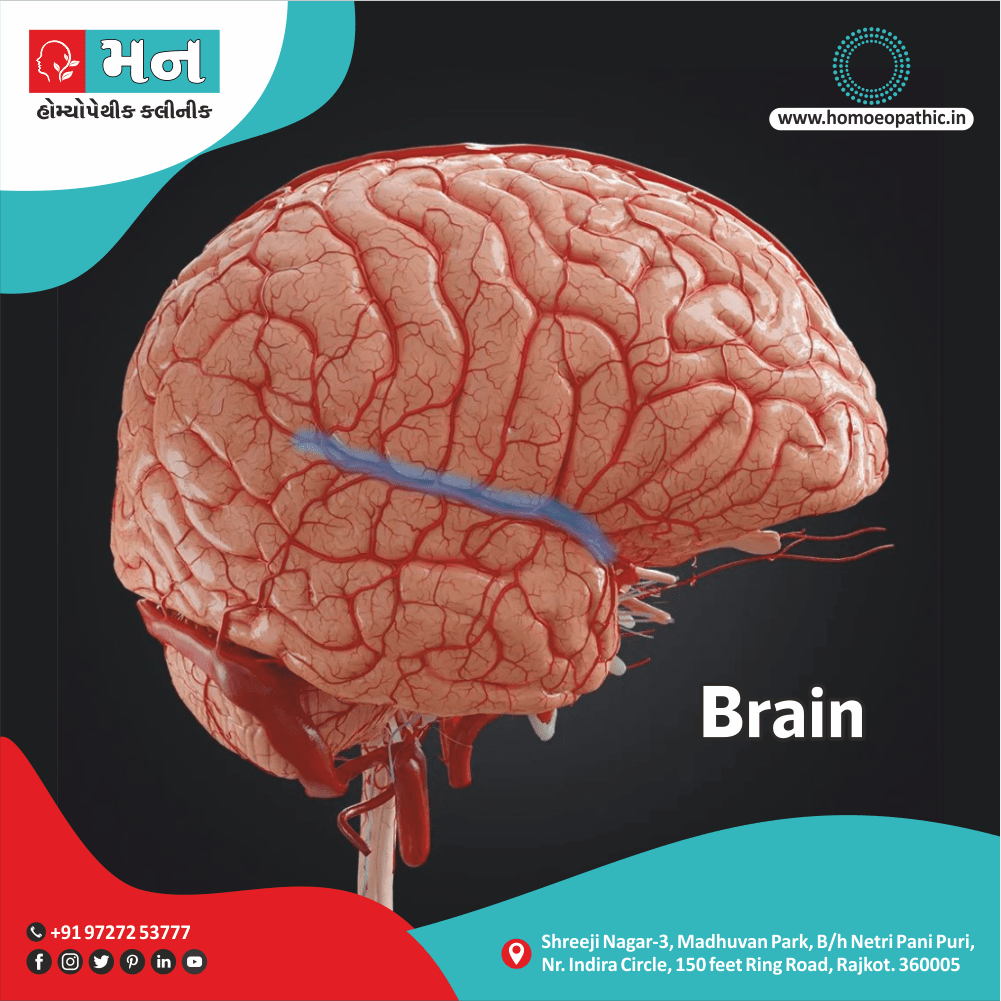
- Dementia is a symptom of a variety of specific structural brain diseases as well as several system degenerations.
- Alzheimer’s disease presently is the commonest cause in the developed world, causing a cortical-subcortical degeneration of ascending cholinergic neurons and large pyramidal cells in the cerebral cortex.
- Clinically, the disease reflects predominantly deterioration of function in the association cortex.
- Pharmacologically and pathologically, abnormalities are more diffuse and extend into sensorimotor cortical areas as well. (6)
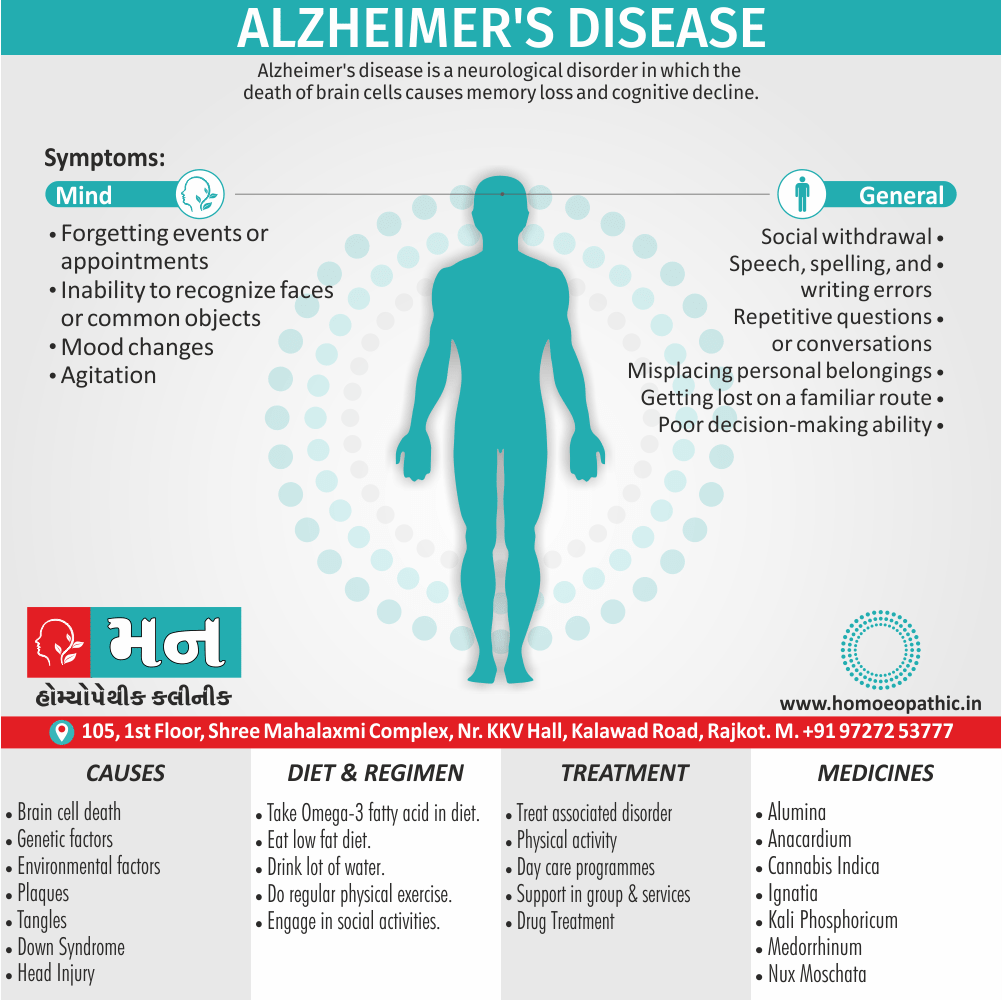
1.Alzheimer’s Dementia:
This is the commonest cause of dementia, seen in about 70% of all cases of dementia in USA. It is more commonly seen in women. Earlier, it was differentiated into two forms: a presenile form and a senile
form. Autopsy shows macroscopic changes such as enlarged cerebral ventricles, widened cerebral sulci and shrinkage of cerebral cortex.
Neurochemically, there is a marked decrease in brain choline acetyltransferase (in other words, CAT) with a similar decrease in brain acetylcholinesterase (AchE).
Treatment:
Cholinesterase Inhibitors:
- Rivastigmine(1.5 mg twice a day to 6 mg twice a day).
- Donepezil(5-10 mg/day).
- Galantamine (4 mg twice a day to 12 mg twice a day) have used in the recent past for treatment of moderate dementia with Alzheimer’s disease.
These elevate acetylcholine (Ach) concentrations in cerebral cortex by slowing the degradation of acetylcholine released by still intact cholinergic neurons in Alzheimer’s disease.
Memantine (5-20 mg/day), an N-methyl-D’Aspartate (NMDA) antagonist, is also available for the treatment of moderately severe to severe Alzheimer’s disease.
2. Multi-infarct Dementia:
Multi-infarct dementia is the second commonest cause of dementia, seen in 10-15% of all cases, though it is probably more common in India. Occurrence of multiple cerebral infarctions can lead to a progressive disruption of brain function, leading to dementia.
The most typical form of multi-infarct dementia is characterised by the following features:
1. An abrupt onset.
2. Acute exacerbations (due to repeated infarct ions).
3. Stepwise clinical deterioration (especially, step-ladder pattern).
4. Fluctuating course.
5. Presence of hypertension (most commonly) or any other significant cardiovascular disease.
6. History of previous stroke or transient ischemic attacks (in other words, TIAs).
Diagnosis: Emotional lability is common. EEG (specifically, showing focal area of slowing) and brain imaging (either CT scan or MRI scan of brain showing multiple infarcts) help in diagnosis.
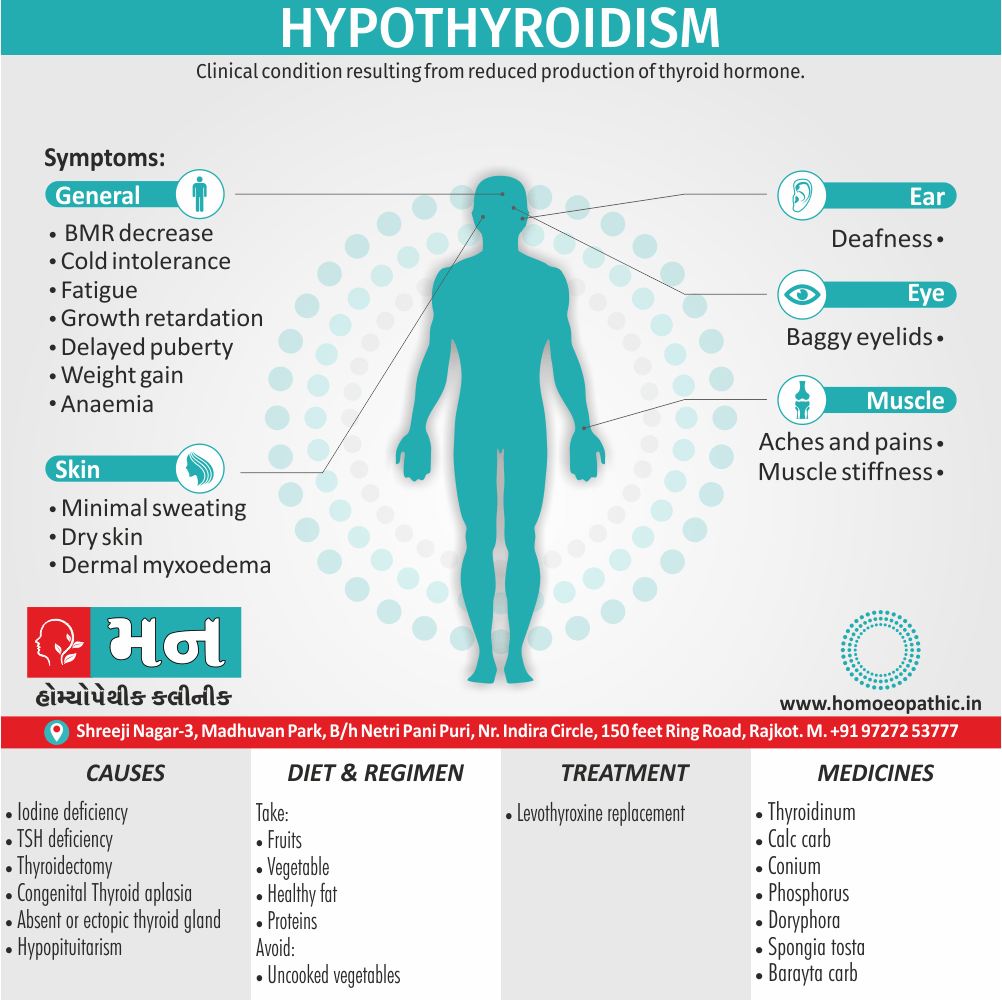
3. Hypothyroid Dementia:
This has been considered one of the most important treatable also reversible causes of dementia, second only to toxic dementias.
Although it accounts for less than 1% of dementias, hypothyroidism should be suspected in every patient of dementia.
All in all, Prompt treatment can reverse the dementing process and can lead to complete recovery if the treatment is start within two years of the onset of dementia.
4. AIDS Dementia Complex:
About 50-70% of patients suffering from AIDS exhibit a triad of cognitive, behavioural and motoric deficits of subcortical dementia type and this is known as the AIDS-dementia complex (in other words, ADC).
As the AIDS virus (a lentivirus, a type of retrovirus) is highly neurotropic and the virus crosses the blood-brain barrier early in the course of the disease cognitive impairment is nearly ubiquitous in AIDS.
Diagnosis: The diagnosis is established by ELISA (enzyme linked immunosorbent assay) showing anti-HIV antibodies, and the Western Blot test (blotting of antibody specificities to HIV-specific proteins).
A Cranial CT scan can show cortical atrophy 1-4 months before the onset of clinical dementia while MRI scan is helpful in detecting the white matter lesions.
5. Lewy Body Dementia:
Lewy body dementia is now believe to be the second most common cause of the degenerative dementias, accounting for about 4% of all dementias.
Typically, the clinical features of Lewy body dementia include:
i. Fluctuating cognitive impairment over weeks or months, with involvement of memory and higher cortical functions (such as language, visuo-spatial ability, praxis and reasoning). Lucid intervals can be present in between fl uctuations.
ii. Recurrent and detailed visual hallucinations.
iii. Spontaneous extrapyramidal or parkinsonian symptoms such as rigidity and tremors.
iv. Neuroleptic sensitivity syndrome, characterised by a marked sensitivity to the effects of typical doses of antipsychotic drugs (resulting in severe extrapyramidal side-effects with use of antipsychotics).
Other clinical features:
It may include repeated falls, autonomic dysfunction (e.g. orthostatic hypotension), urinary incontinence, delusions and depressive features.
Although Lewy bodies (intracytoplasmic inclusion bodies) are also present in Parkinson’s disease, the occurrence of Lewy bodies in Lewy body dementia is more widespread. Antipsychotic medication should be avoided (or used with extreme caution and in low doses) in patients with Lewy body dementia.
Diagnosis: A PET (Positron Emission Tomography) or SPECT (Single Photon Emission Computerised Tomography) scan of brain may show low dopamine transporter uptake in basal ganglia. [2]
Cognition such as:
- Poor memory
- Impaired attention
- Aphasia, agnosia, and apraxia
- Disorientation
- ‘Personality change’
Behaviour such as:
- Odd and disorganized
- Restless, wandering
- Self-neglect
- Disinhibition
- Social withdrawal Mood
Anxiety i.e.:
- Anxiety
- Depression
Thinking i.e.:
- Slow, impoverished
- Delusions
Perception such as:
- Illusions
- Hallucinations
Insight such as:
- Impaired. [1]
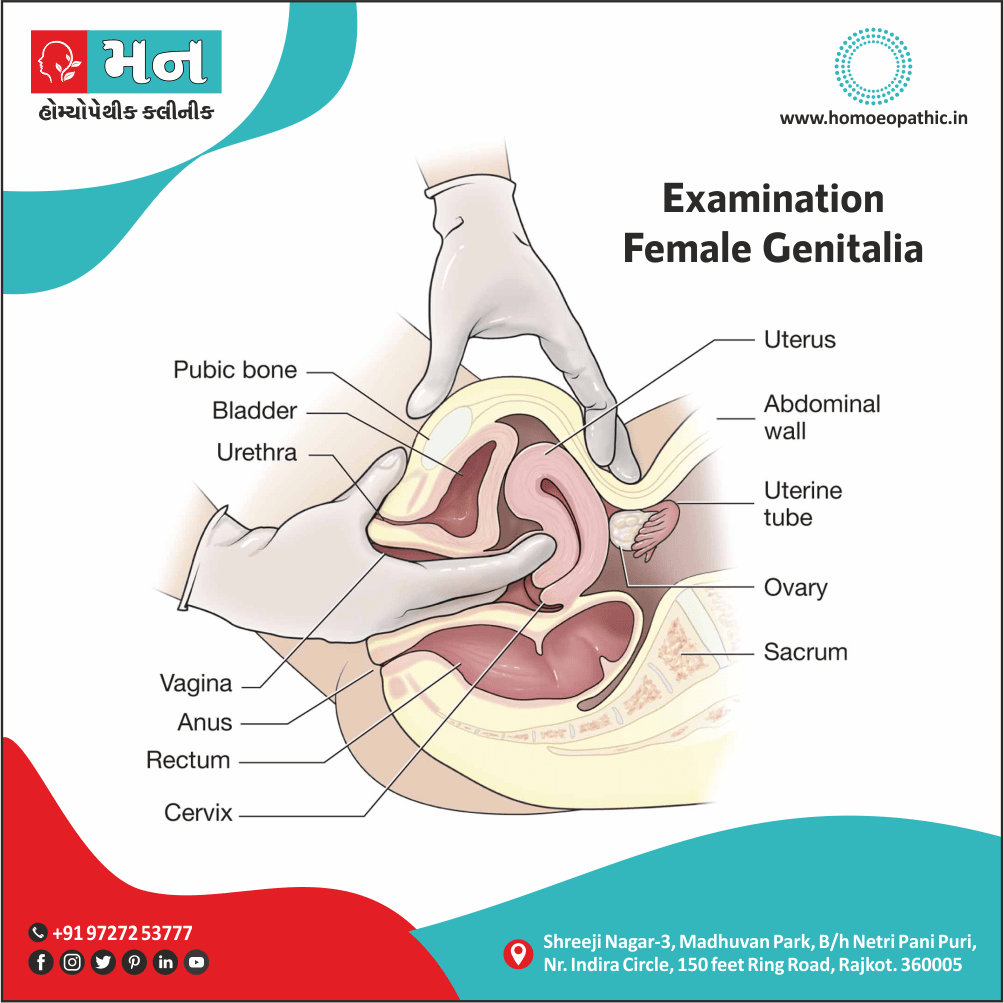
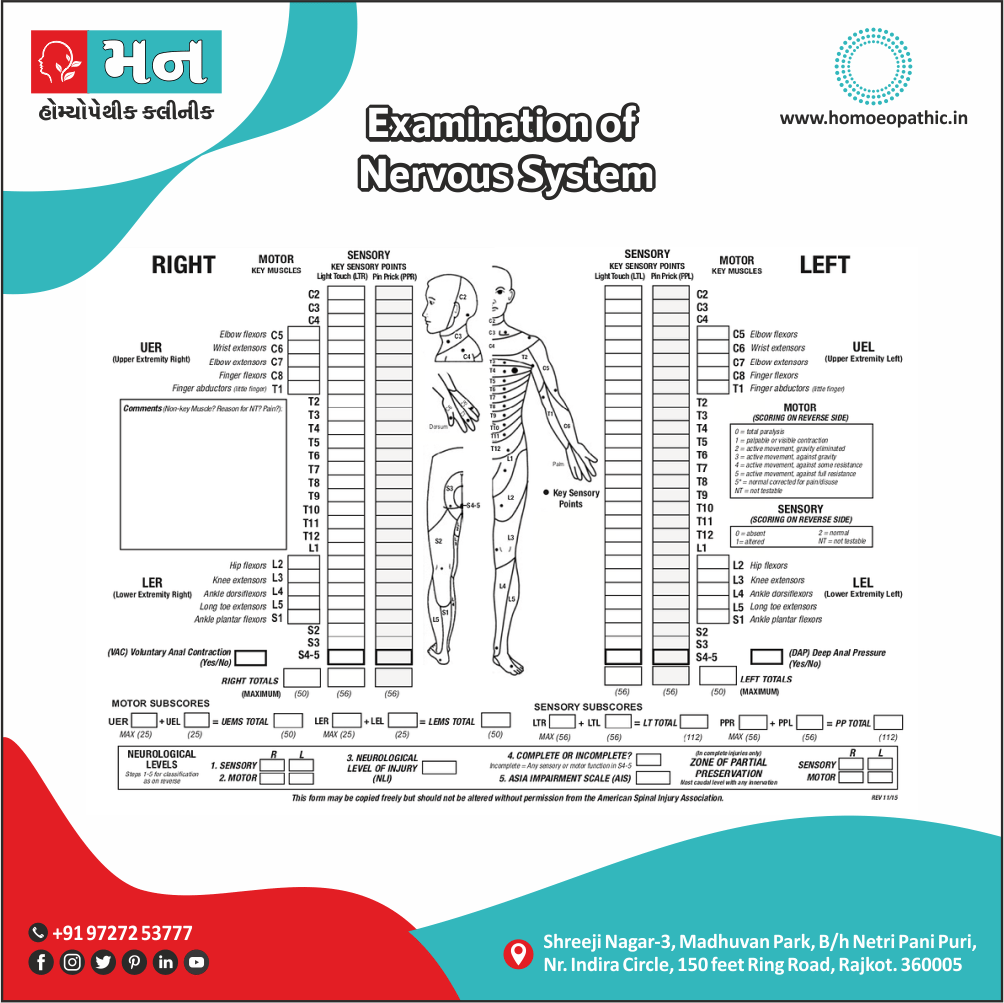
Clinical examination of Dementia
A thorough general physical examination followed by focused focal neurologic deficits examination that may be consistent with prior strokes, parkinsonism (rigidity and/or tremors), gait abnormalities or slowing, and eye movements should be preferably done. Some patients with Alzheimer disease (AD) generally have no motor or sensory deficits at presentation.
The final diagnosis of dementia is made on the basis of the clinical picture, increasingly with neuroimaging results for backup. For research purposes, the diagnosis depends on both a clinical diagnosis and a pathological diagnosis (i.e., based on the examination of brain tissue, usually from autopsy).
Proper differential diagnosis between the types of dementia (see below) will require, at the least, referral to a specialist, e.g. a geriatric internist, geriatric psychiatrist, neurologist, neuropsychologist or gero psychologist. However, there are some brief (5-15 minutes) tests that have good reliability and can be used in the office or other setting to evaluate cognitive status. Examples of such tests include the abbreviated mental test score (AMTS), the mini mental state examination (MMSE), Modified Mini-Mental State Examination (3MS), the Cognitive Abilities Screening Instrument (CASI and the clock drawing test.
An AMTS score of less than six (out of a possible score of ten) and an MMSE score under 24 (out of a possible score of 30) suggests a need for further evaluation. Scores must be interpreted in the context of the person’s educational and other background, and the particular circumstances (for example, a person in great pain will not be expected to do well on many tests of mental ability). (6)
Investigation of Dementia
Laboratory Investigations:
- Basic Haematology
- Biochemistry
- Liver function
- Thyroid function
- Vitamin B12
- Folate
- Thiamine
- Calcium
- Glucose.
Imaging:
- A CT or MRI brain scan may be needed, as they are valuable in the diagnosis of both focal and diffuse cerebral pathology. [1]
- Focused history, mental status examination, and functional assessment.
- Measurement of the protein 14-3-3 in cerebrospinal fluid (CSF)
- CSF concentrations of tau protein and beta-amyloid peptide 42
According to ICD-10, the following features are required for diagnosis:
- Evidence of;
Decline in both memory and thinking, sufficient enough to impair personal activities of daily living
Memory impairment (typically affecting registration, storage, and retrieval of new information though previously learned material may also be lost particularly in later stages.
Impaired thinking, presence of clear consciousness (consciousness can be impaired if delirium is also present), and a duration of at least 6 months. [2]
- The Mini Mental State Examination (MMSE) is used widely in assessment; it combines standard questions with tests of spatial ability, and has high sensitivity and specificity. [2]
Differential diagnosis of dementia
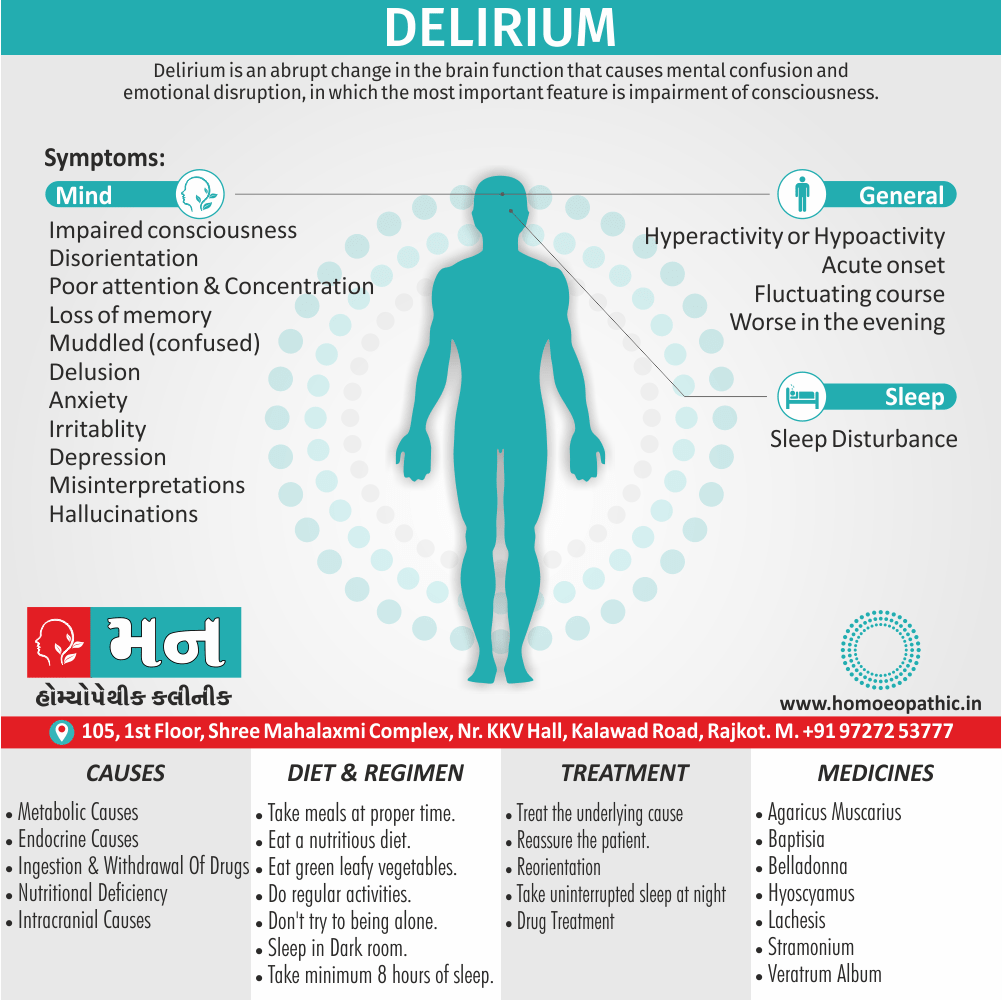
- Delirium
- Depression
- Amnestic disorders
- Aphasias
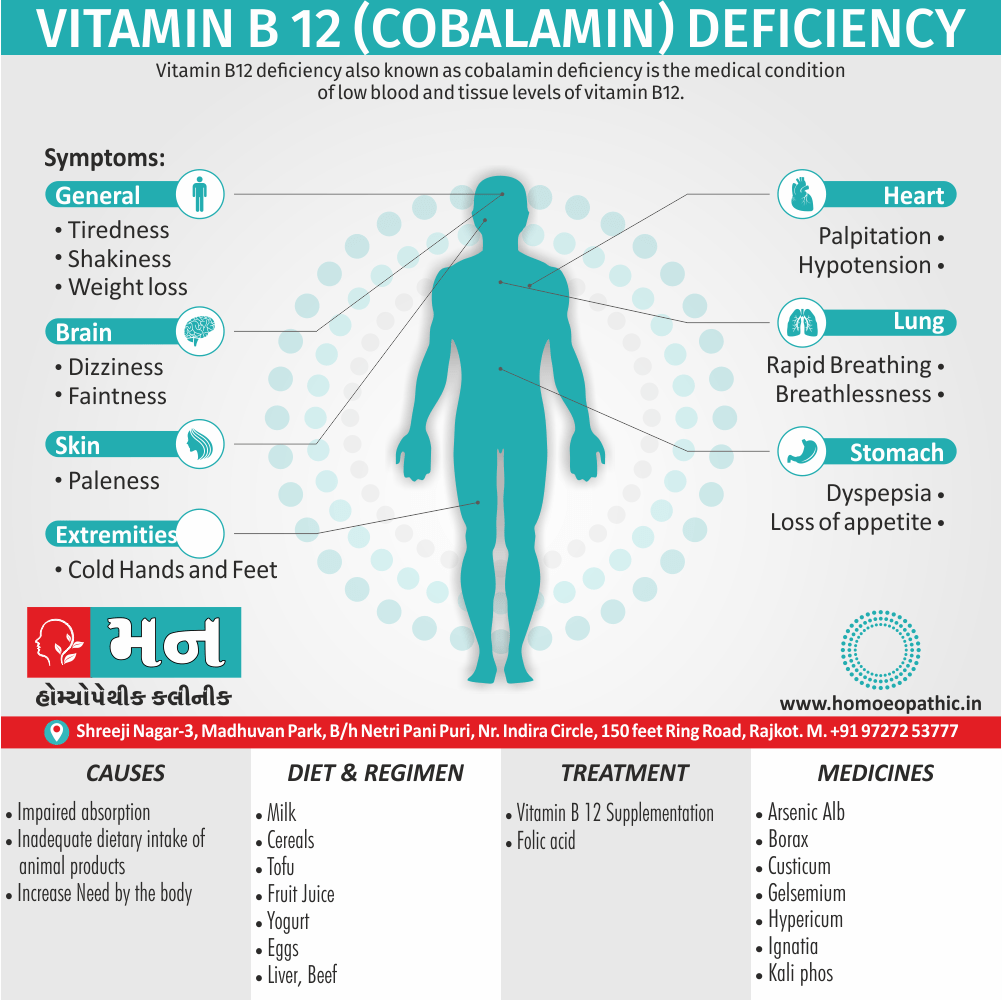
- Vitamin B12 deficiency
- Vitamin B6 deficiency
- Thiamine deficiency
- Parkinson’s disease
- Marijuana abuse
- Vascular dementia
- AIDS. (6)
General measures:
- Treat any physical disorders
- Psychoeducation of patient, family, also carers
- Promote and maintain independence with a written care plan
- besides this, Provide training courses and support groups for carers
- Respite care
- Lastly, Palliative care input
Psychological:
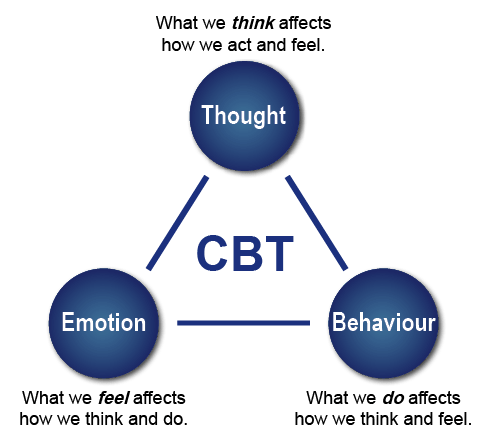
- Structured group cognitive stimulation programme
- For agitation: For example; aromatherapy, dance/music therapy, animal therapy
- Psychological support for carers
Pharmacological:
- Acetylcholinesterase inhibitors: (e.g. Donepezil, Galantamine, Rivastigmine) increase the concentration of and duration of action of acetylcholine in the central nervous system. Additionally, There is evidence that in moderately severe Alzheimer’s disease, these drugs improve cognitive function and behaviour for up to a year. All in all, these drugs should only be prescribed by specialists, and should be stopped after 6 months if there is no clinical benefit.
- Memantine: It is a glutamine NMDA receptor antagonist which improves cognition, mood, and behaviour in moderate to severe Alzheimer’s.
- For agitation such as:
Antipsychotics : Antipsychotics should generally be avoided whenever possible and only have a role in patients with severely distressing symptoms or agitation causing risk to self or others.
They should be avoided in those with mild to moderate dementia, as there is a slight increase in the risk of cerebrovascular events.
The recommended drugs are haloperidol also olanzapine. A few patients need long-term oral antipsychotics to manage their behaviour at home.
Benzodiazepines: Benzodiazepines should be avoided wherever possible, especially during the day.
Intramuscular lorazepam is a suitable alternative to an antipsychotic for extreme agitation, also should be tried if antipsychotics do not relieve the symptoms.
- For depression: e.g. antidepressants. [1]
Prevention of Dementia
Exercise
- Regular physical activity can help reduce the risk of dementia
Eat well
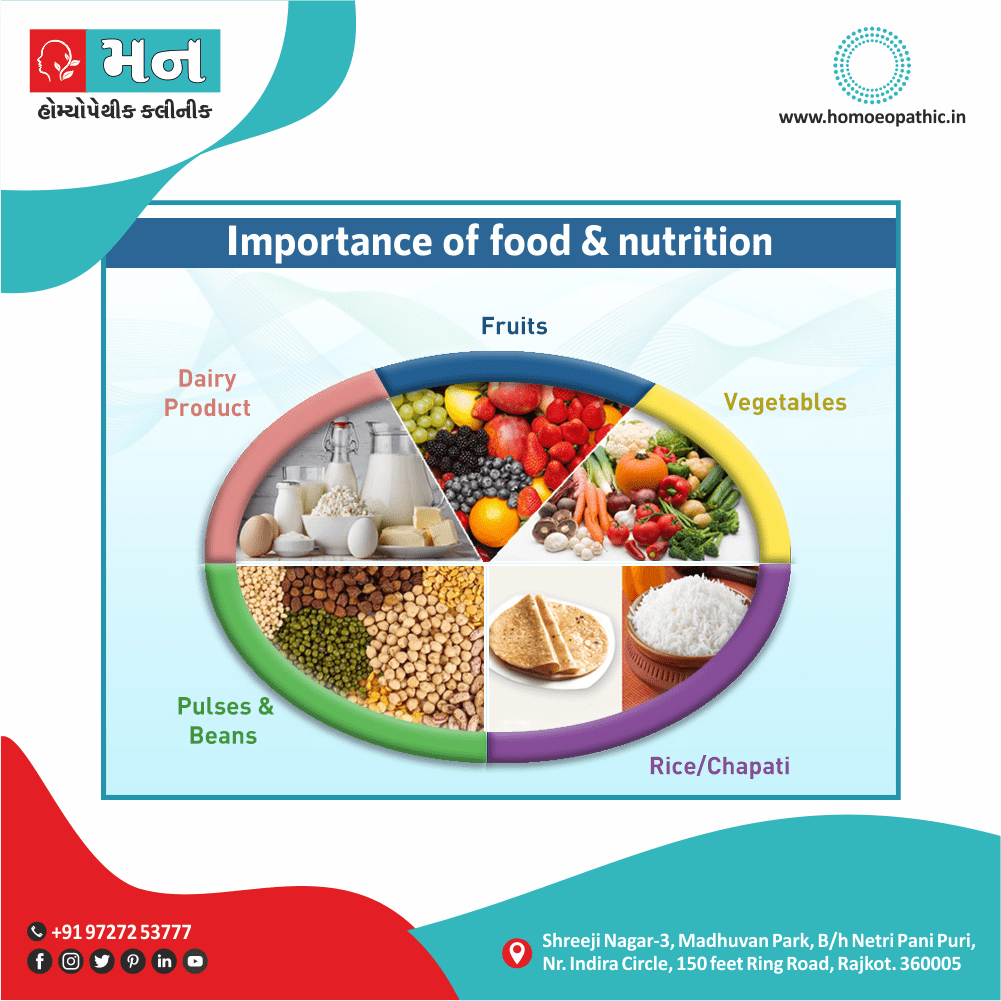
- A diet that’s good for the heart is good for the brain and overall health. A healthy diet may reduce your risk of conditions that can lead to dementia. According to the World Health Organization (WHO), a balanced diet consists of:
- fruit and vegetables
- lentils and beans
- grains, tubers, or roots
- eggs, milk, fish, lean meat
Things to avoid or keep to a minimum are:
- saturated fats
- animal fats
- sugars
- salt
Your diet should center around nutrient-rich, whole foods. Avoid high calorie, processed foods that provide little to no nutritional value.
Don’t smoke
- Research Trusted Source shows that smoking can increase the risk of dementia, especially if you’re 65 years old or more. Smoking affects blood circulation all around your body, including the blood vessels in your brain.
Keep your mind active
An active mind may help lower the risk of dementia, so keep challenging yourself. Some examples would be:
- study something new, like a new language
- do puzzles and play games
- read challenging books
- learn to read music, take up an instrument, or start writing
- stay socially engaged: keep in touch with others or join group activities
- volunteer
Manage overall health
Staying in good shape can help lower risk of dementia, so get a yearly physical. See your doctor if you have symptoms of:
- depression
- hearing loss
- sleep problems
Manage existing health conditions such as:
- diabetes
- heart disease
- high blood pressure
- high cholesterol (7)
Homeopathic Treatment of Dementia
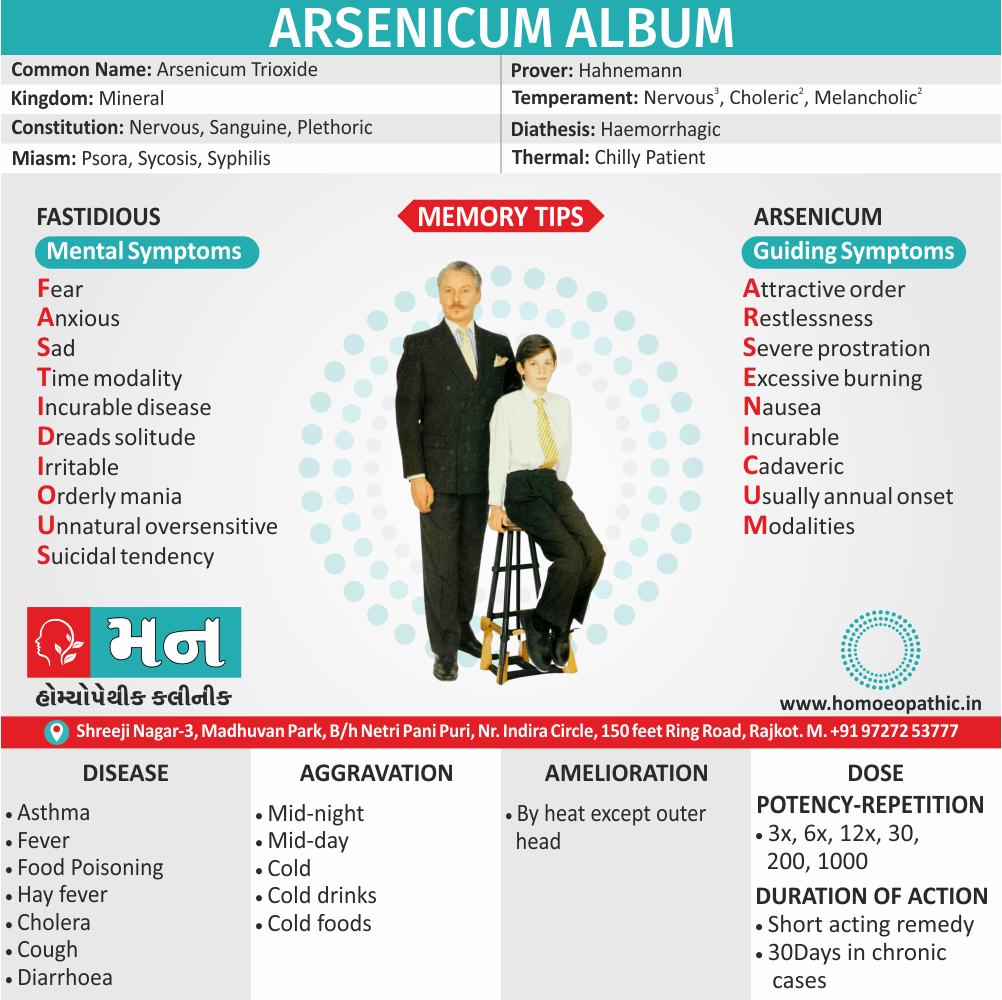
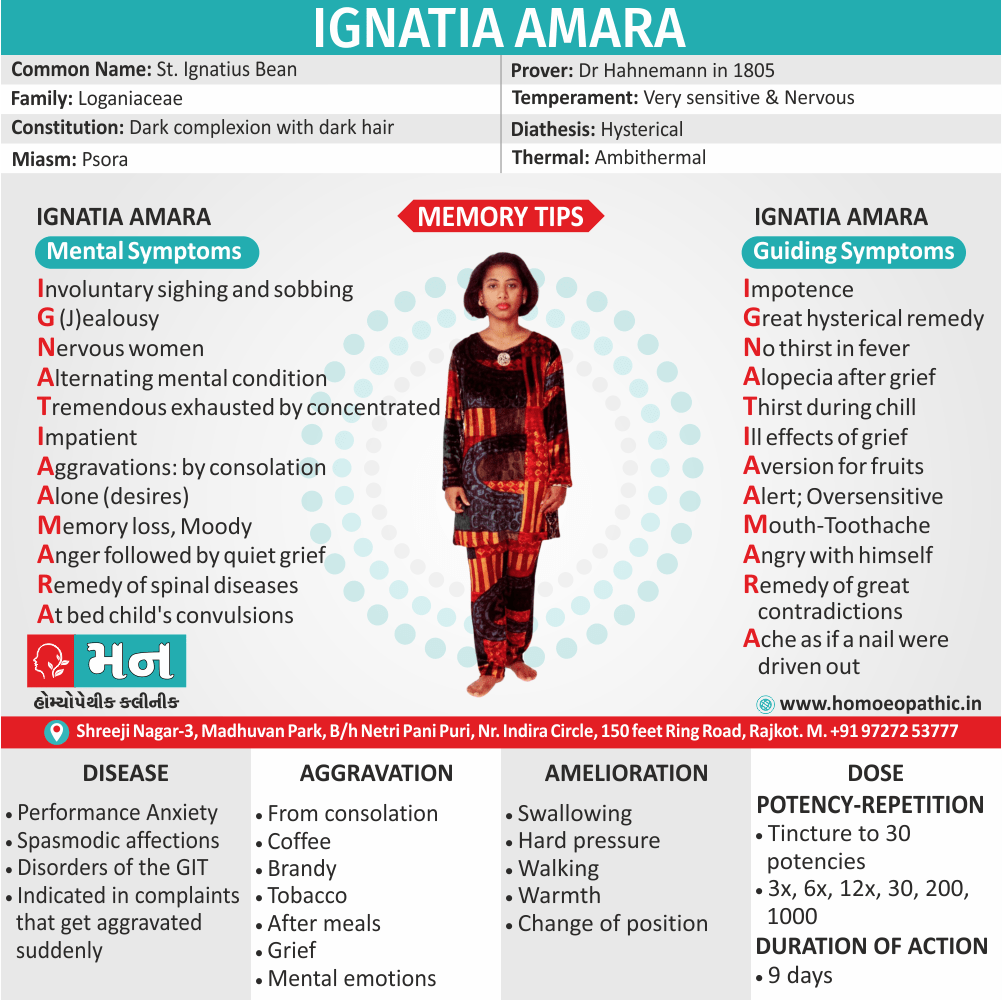
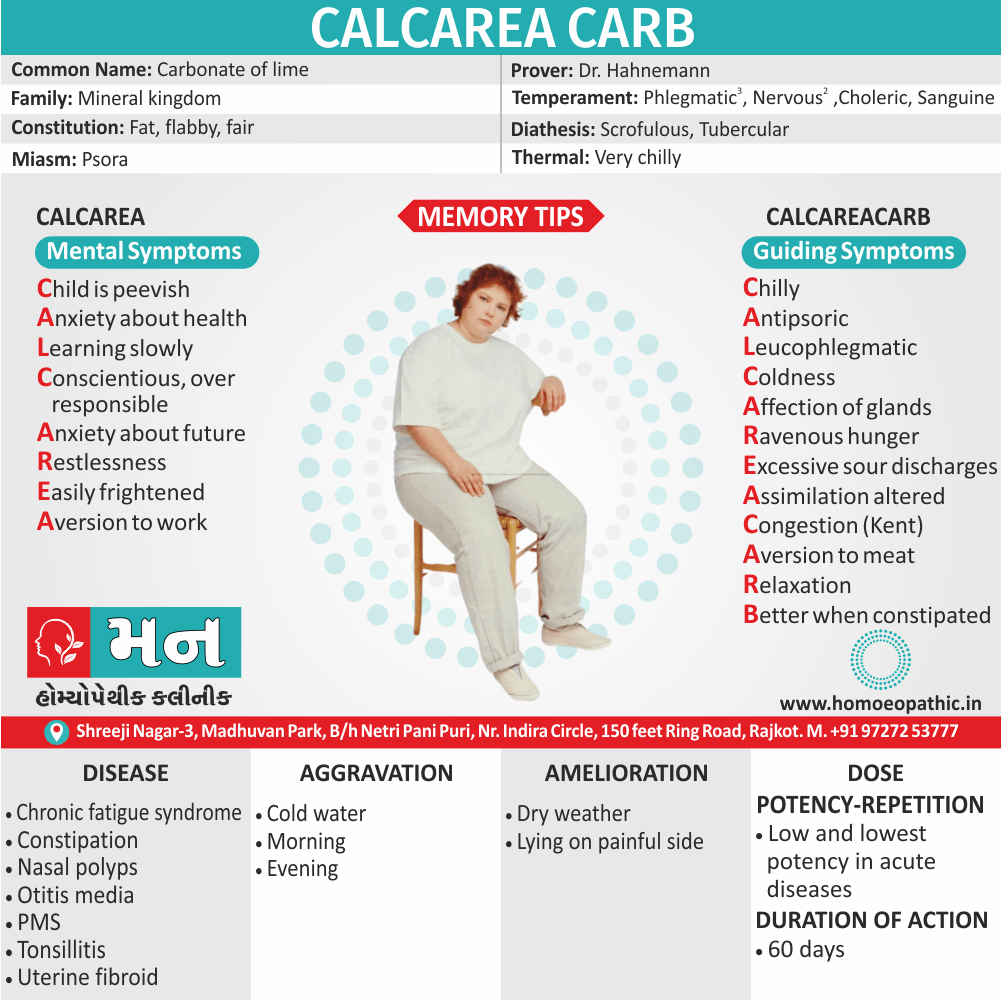
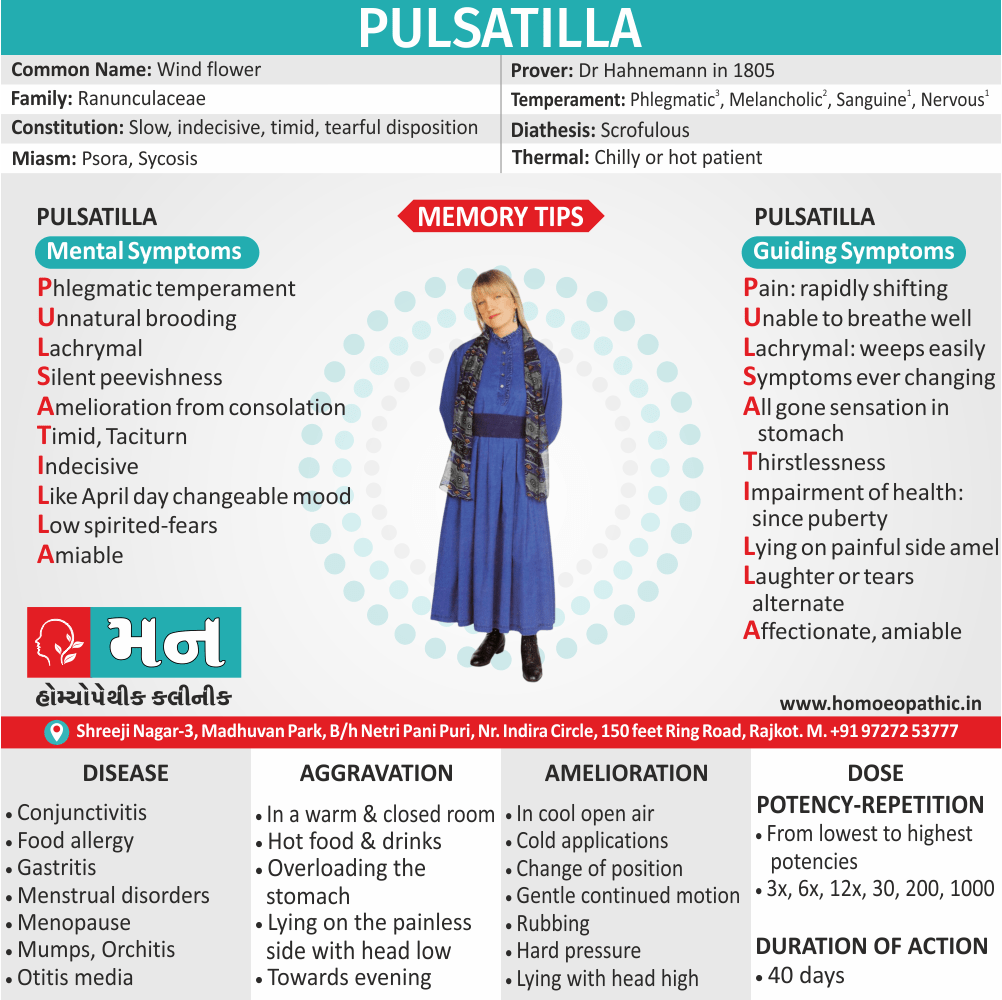
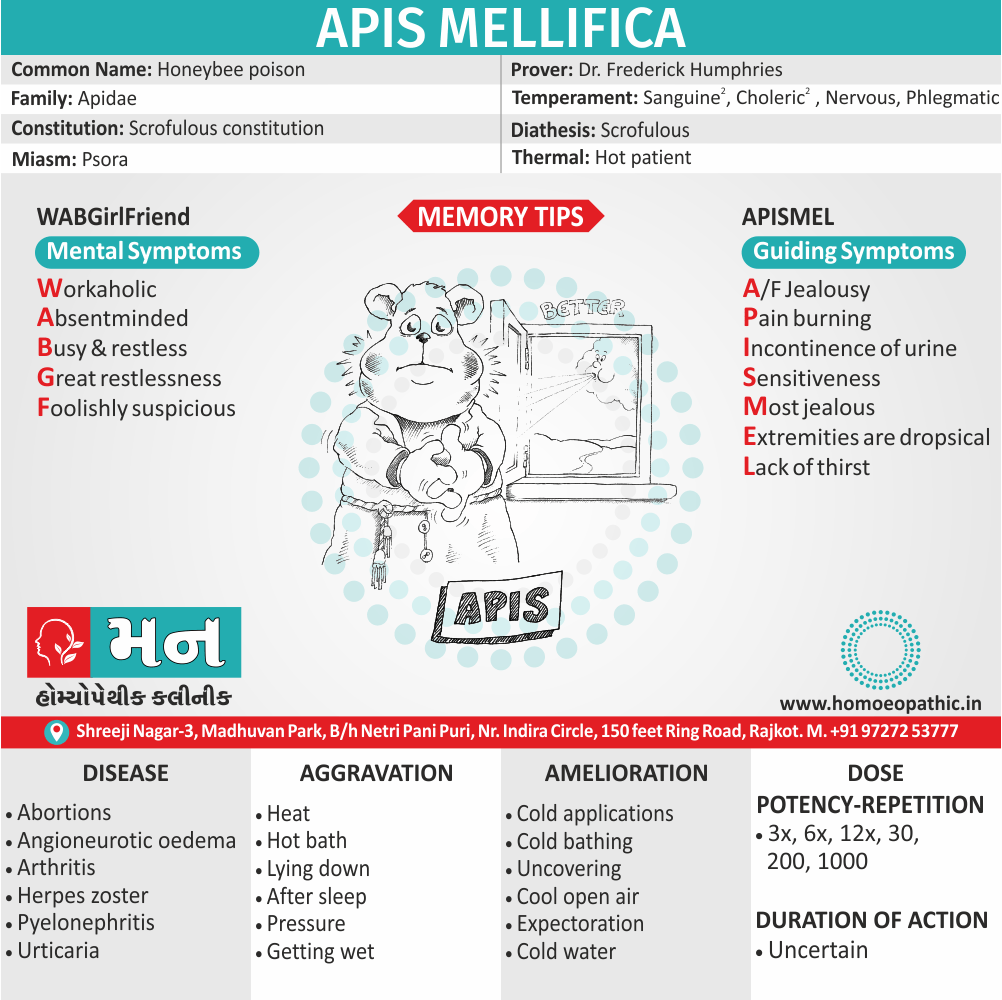
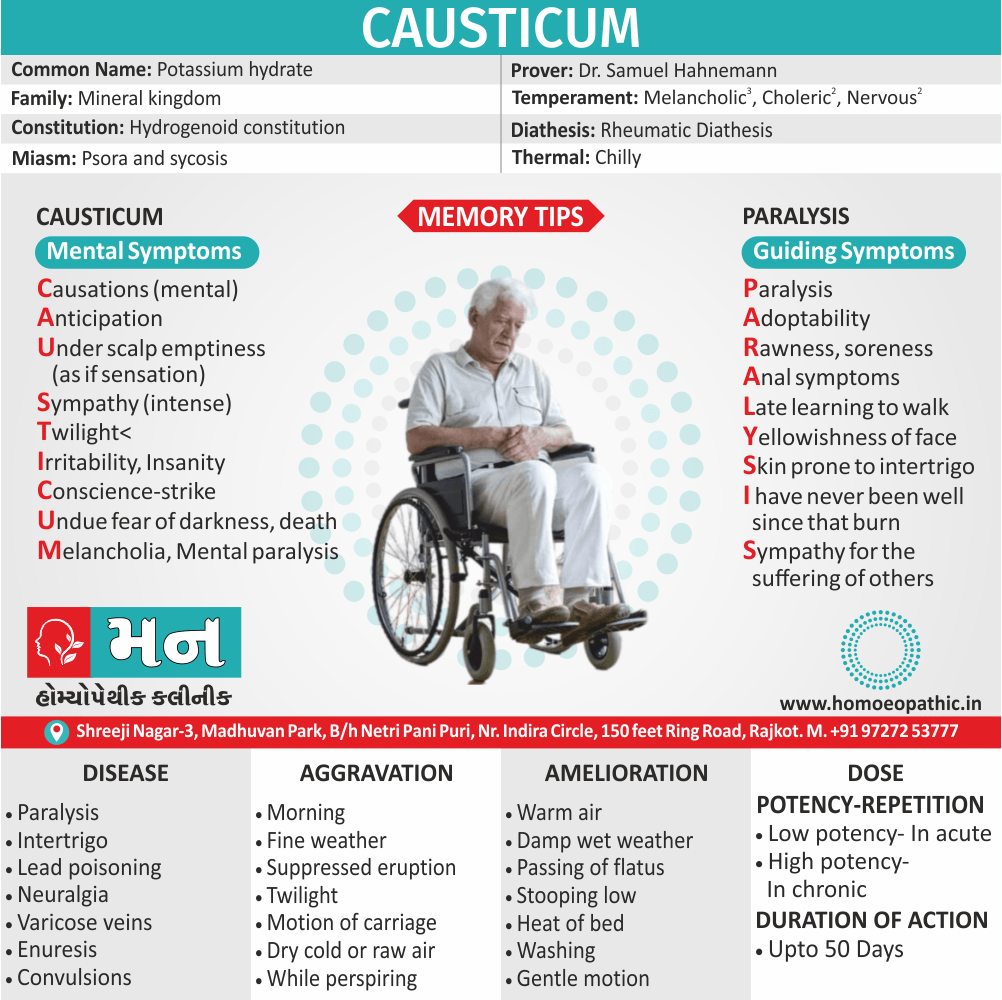
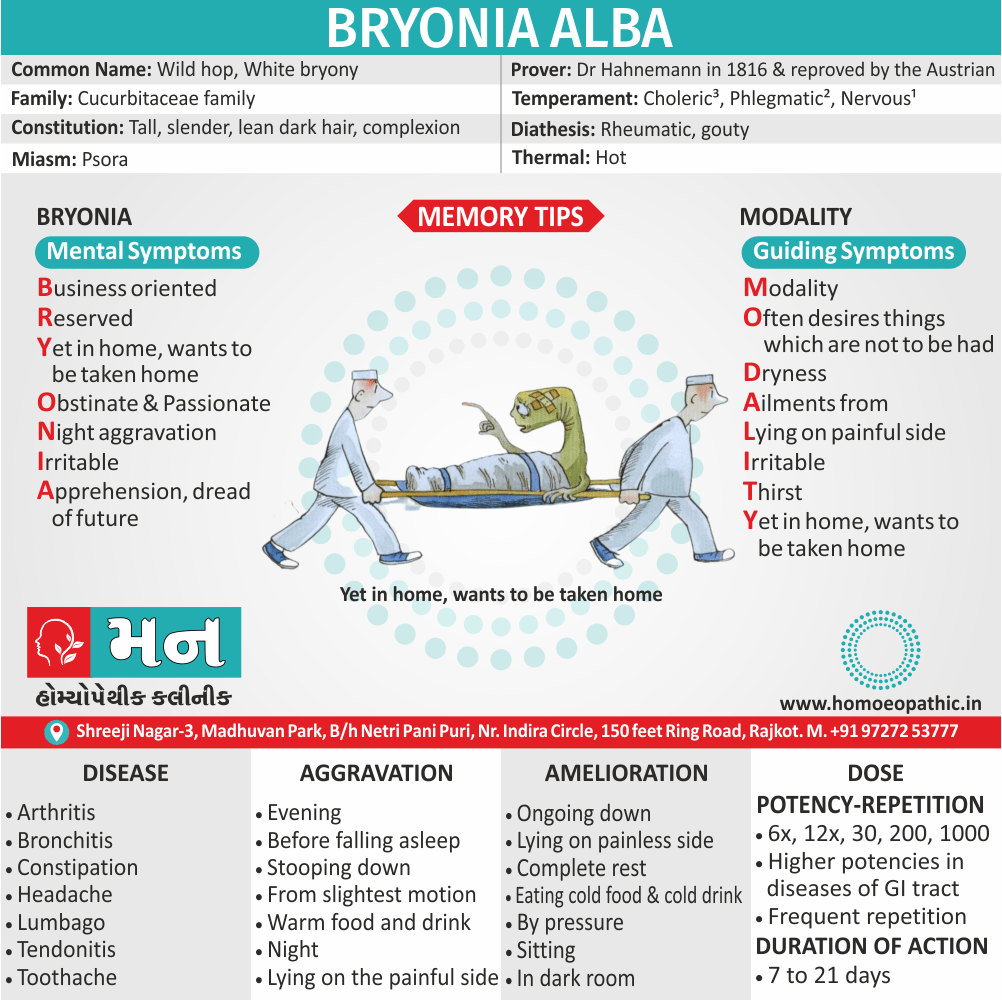
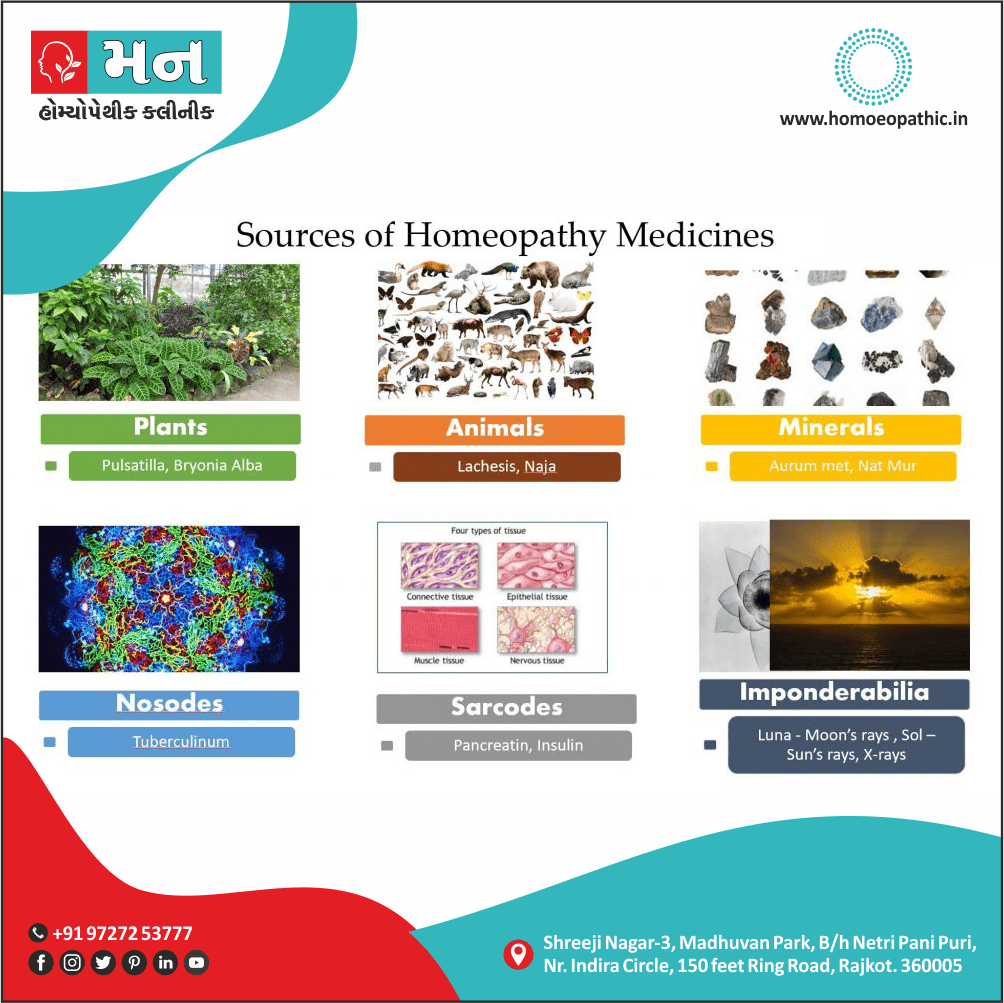
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
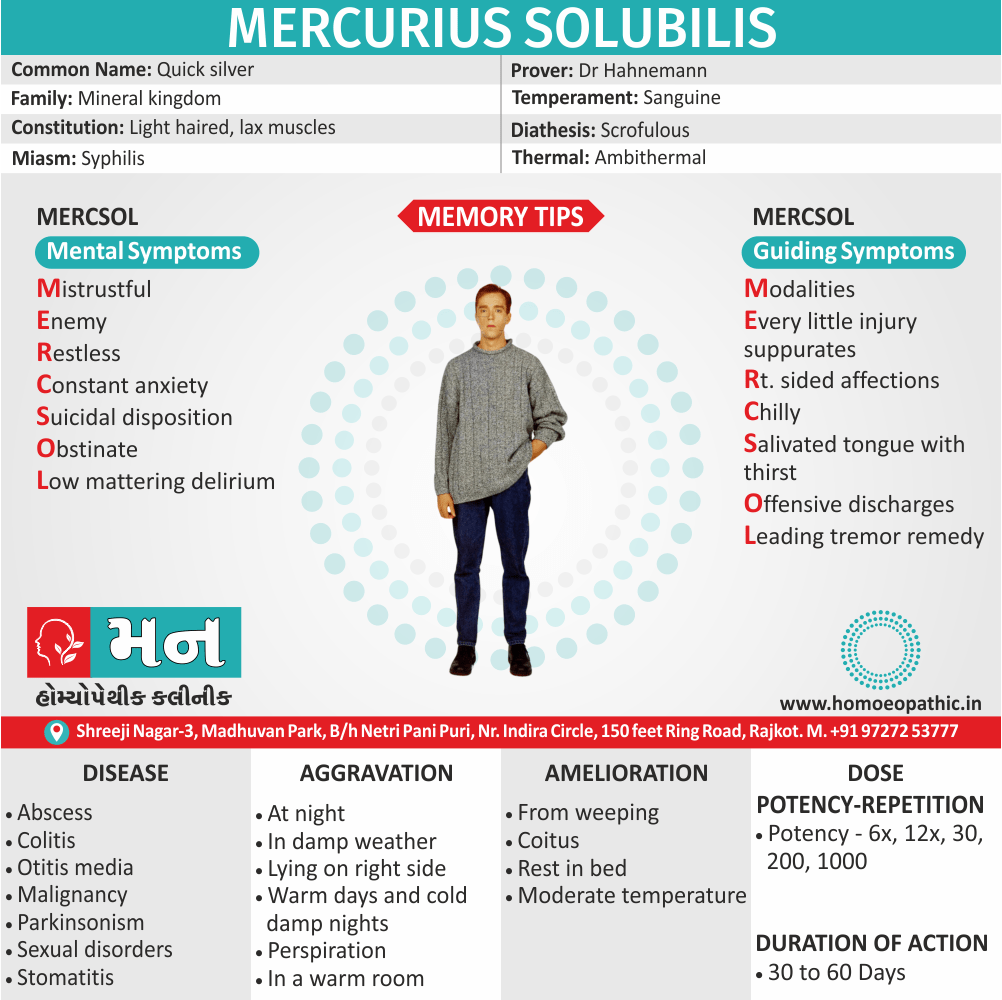
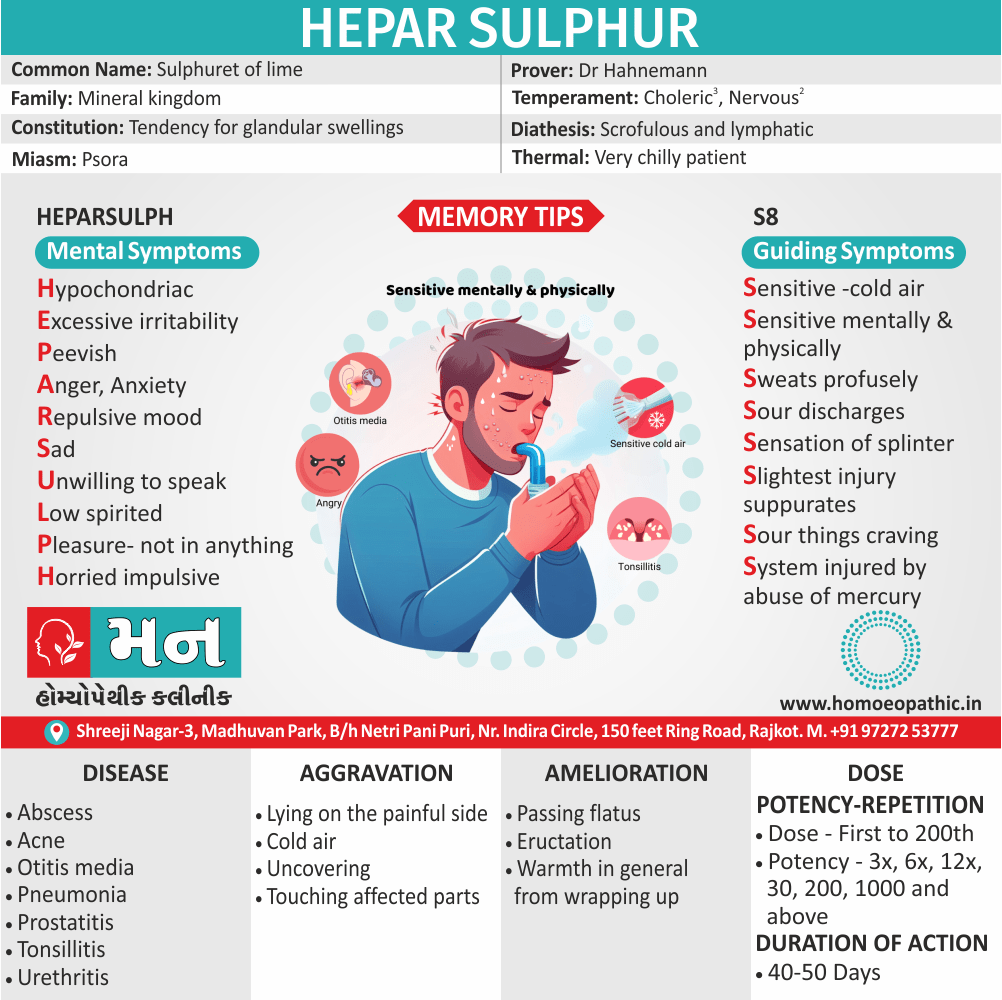
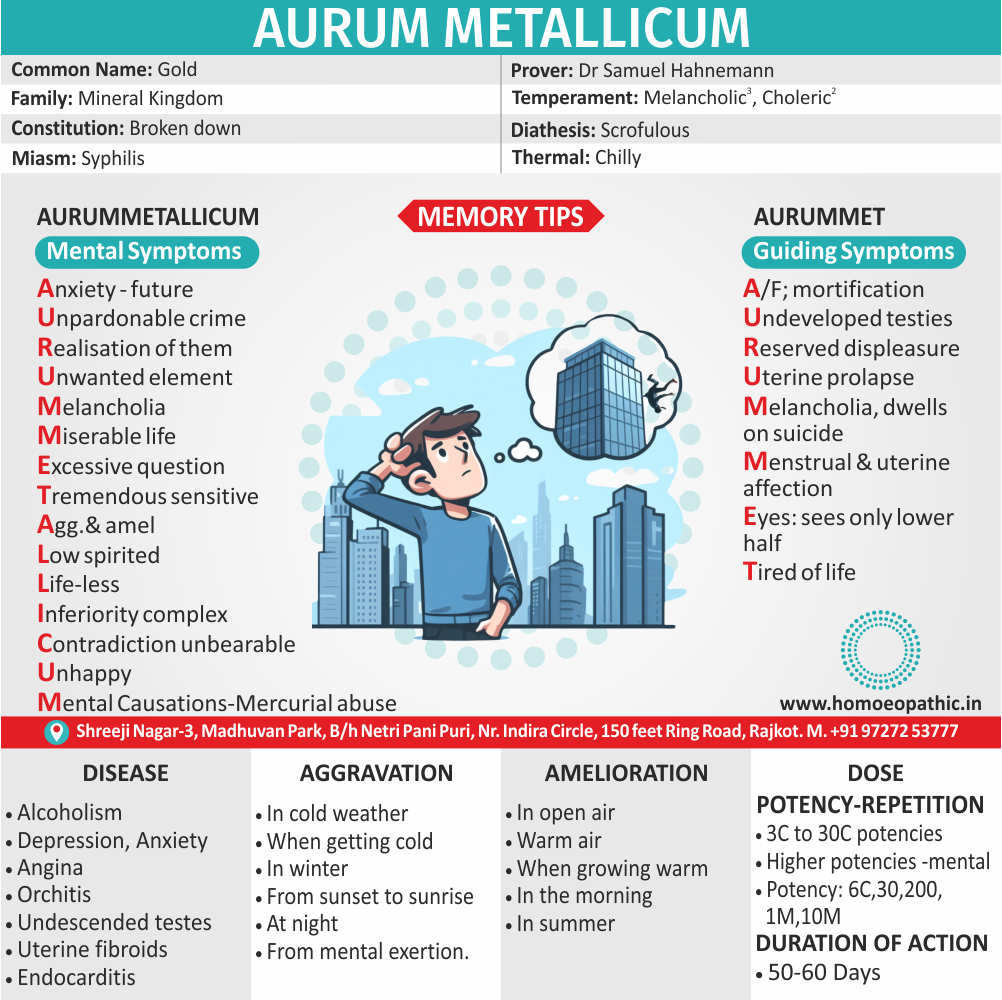
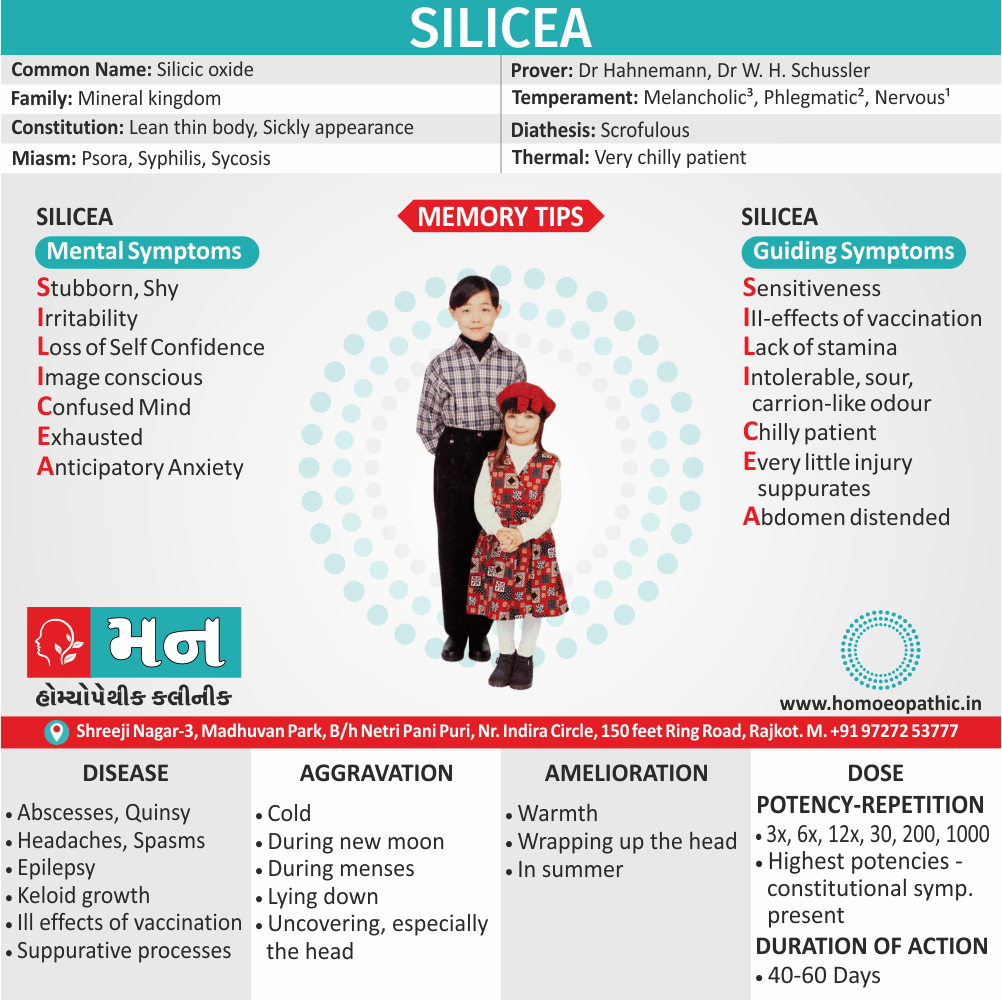
Homeopathic Medicines for Dementia
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
. Anacardium Orientale – A Top Homeopathic Medicine for Dementia
Anacardium Orientale is among the best homeopathic remedies for dementia. Patients needing Anacardium Orientale have impaired memory and marked forgetfulness. The patient suddenly forgets the names of those around and also forgets things he has recently seen. Forgetfulness makes the person low spirited. There is also a marked absent mindedness and a deficiency of ideas. Homeopathy also uses Anacardium Orientale for the treatment of Alzheimer’s.
2. Baryta Carb – A Homeopathic Remedy for Senile Dementia
Baryta Carb is an excellent homeopathic remedy for senile dementia. In such cases, there is progressing mental weakness. There is forgetfulness while speaking and the mind seems clouded. The patient tends to forget the words that he is about to speak. There is a loss of memory, and when the patient tries to recollect past events, he is unable to do so. Baryta Carb works well for the treatment of dementia in the elderly who may have lost mental function after a stroke.
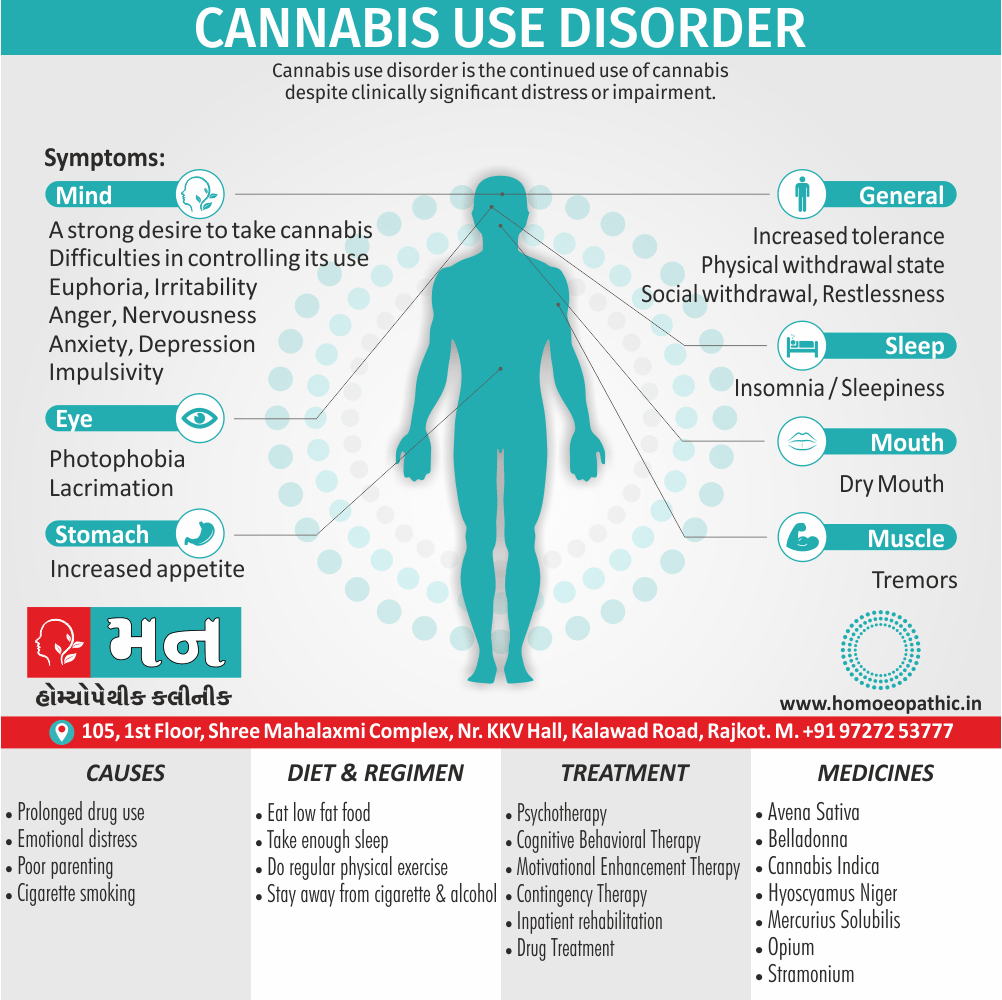
3. Cannabis Indica – Homeopathic Medicine for Dementia with Difficulty in Communication
Cannabis Indica is one of the best homeopathic remedies for dementia in cases where there is difficulty in communication. Cannabis Indica is helpful where a person becomes extremely forgetful while communicating. He forgets the last words spoken by him as well as what he is about to say. He begins to speak a sentence and then suddenly loses the thread of conversation. While writing too, the patient forgets what he intends to write. The mind is foggy, and there is an inability to recall past events. Difficulty in focusing is also experienced.
4. Medorrhinum – Homeopathic Medicine for Dementia Where the Patient Forgets Names and Words
Medorrhinum is a suitable homeopathic medicine for dementia where the person forgets names and words. The main symptom that points to the use of Medorrhinum is forgetting the names of friends and familiar people. The patient may not even remember their own name. There is also forgetfulness while writing, both regarding the words that are to be written as well as their spelling. While speaking, the person may forget the appropriate words. During a conversation, the patient may forget what he was asked; and the question has to be repeated. Along with the above symptoms, there are severe mood changes as well. Happiness alternates with sadness. There is also marked irritability over small things.
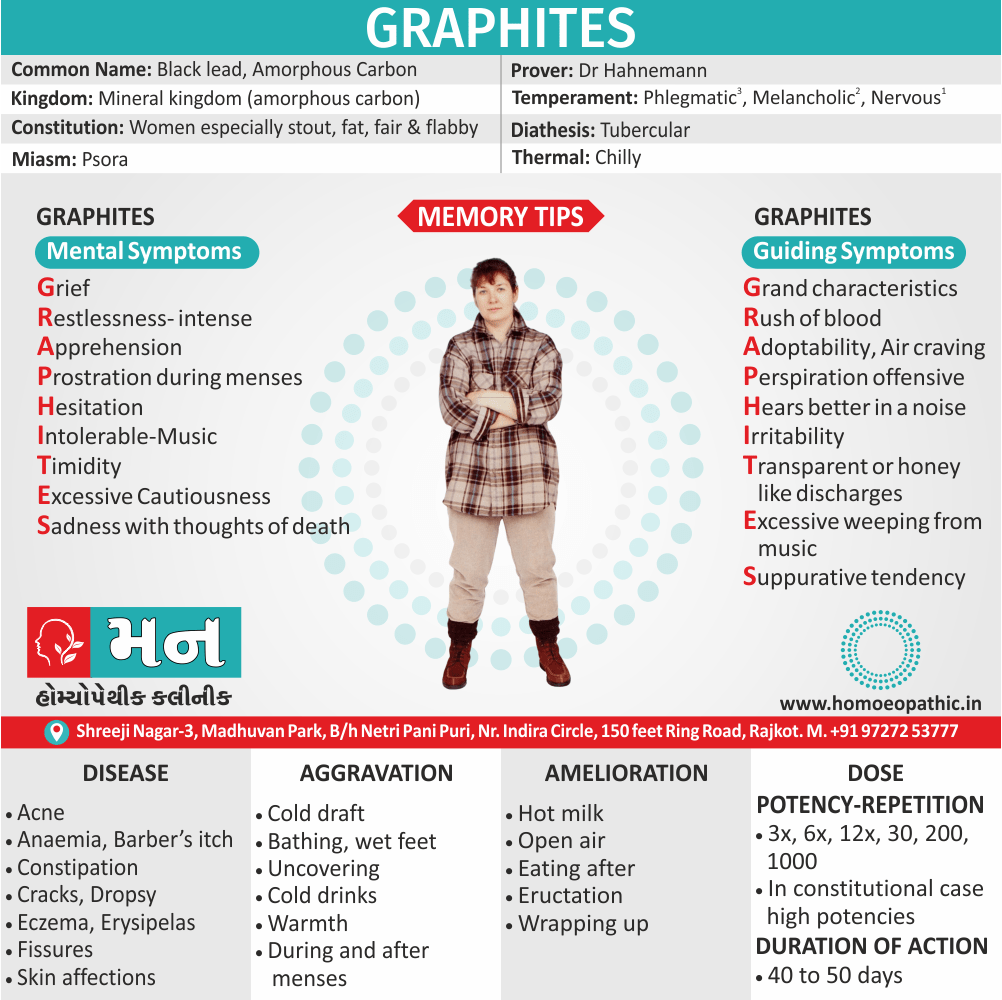
5. Graphites Naturalis – Homeopathic Medicine for Dementia when Indifference Accompanies Memory Loss
Graphites Naturalis is one of the best homeopathic remedies for dementia in cases where indifference accompanies memory loss. The person forgets recent events but remembers past events that occurred at a young age. There is indifference to everything and everybody. Along with this, the patient may be obstinate and moody. Dullness and anxiety, mostly in the mornings, also occur.
6. Kali Phos – A Useful Homeopathic Medicine for Dementia when Prostration Accompanies Memory Loss
Kali Phos is an effective homeopathic medicine for dementia. The main symptom pointing towards the use of Kali Phos is memory loss accompanied by tiredness. There is exhaustion on both mental and physical levels. In such cases, the patient doesn’t recognize his surroundings and is not inclined to speak with others. Sometimes, gloominess, depression, nervousness, and anxiety are also present.
7. Dementia, due to schizophrenia–
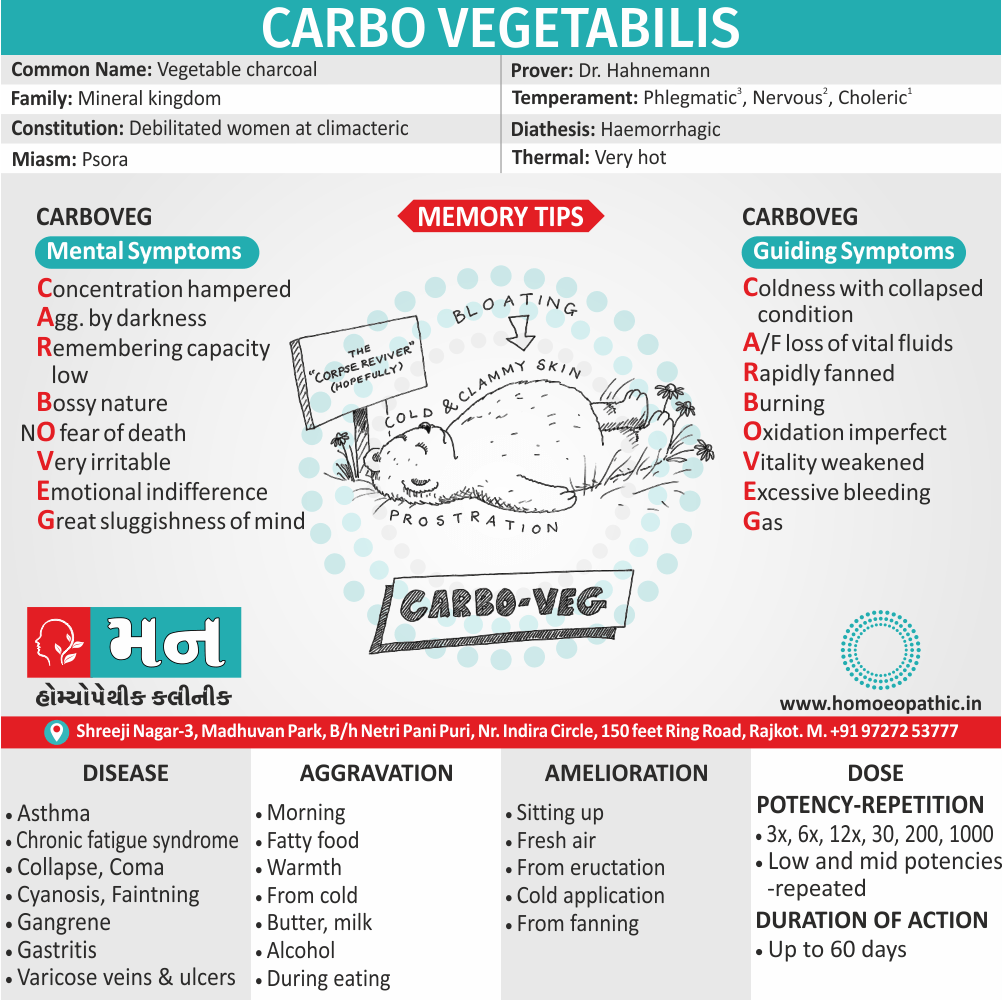
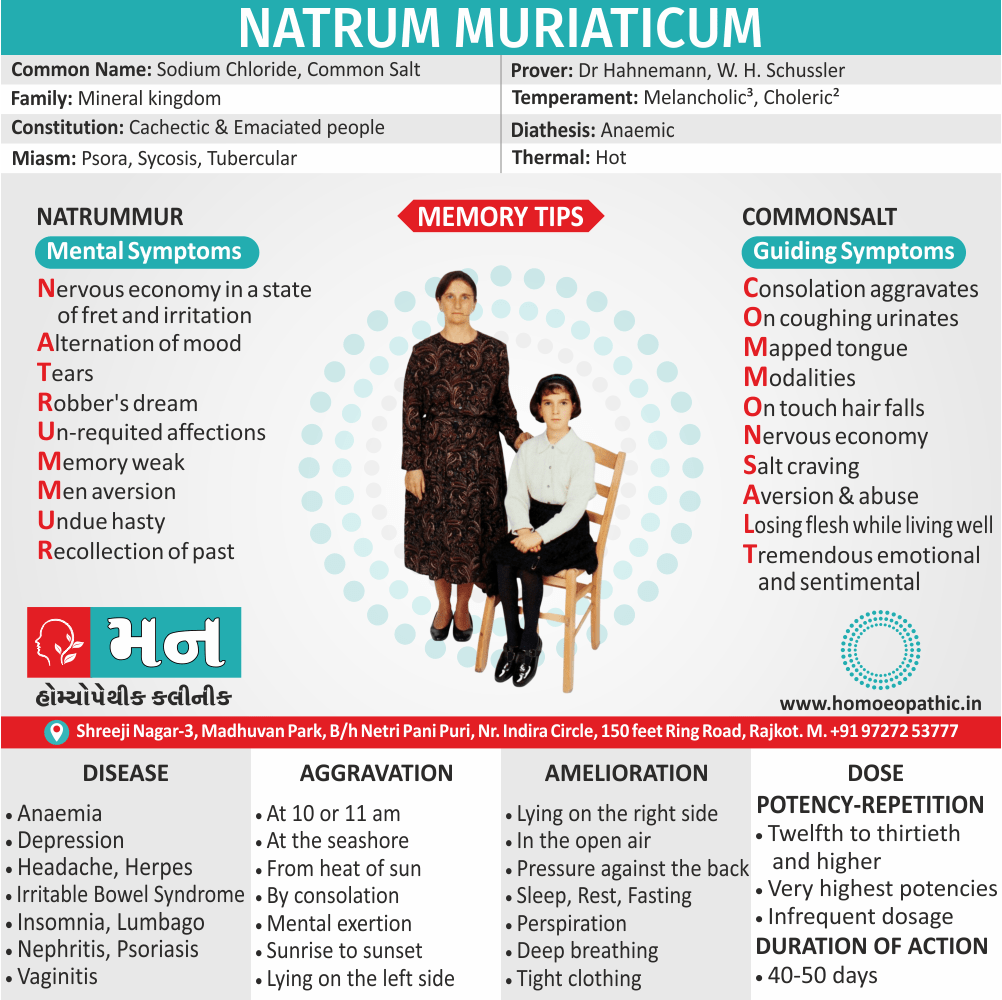
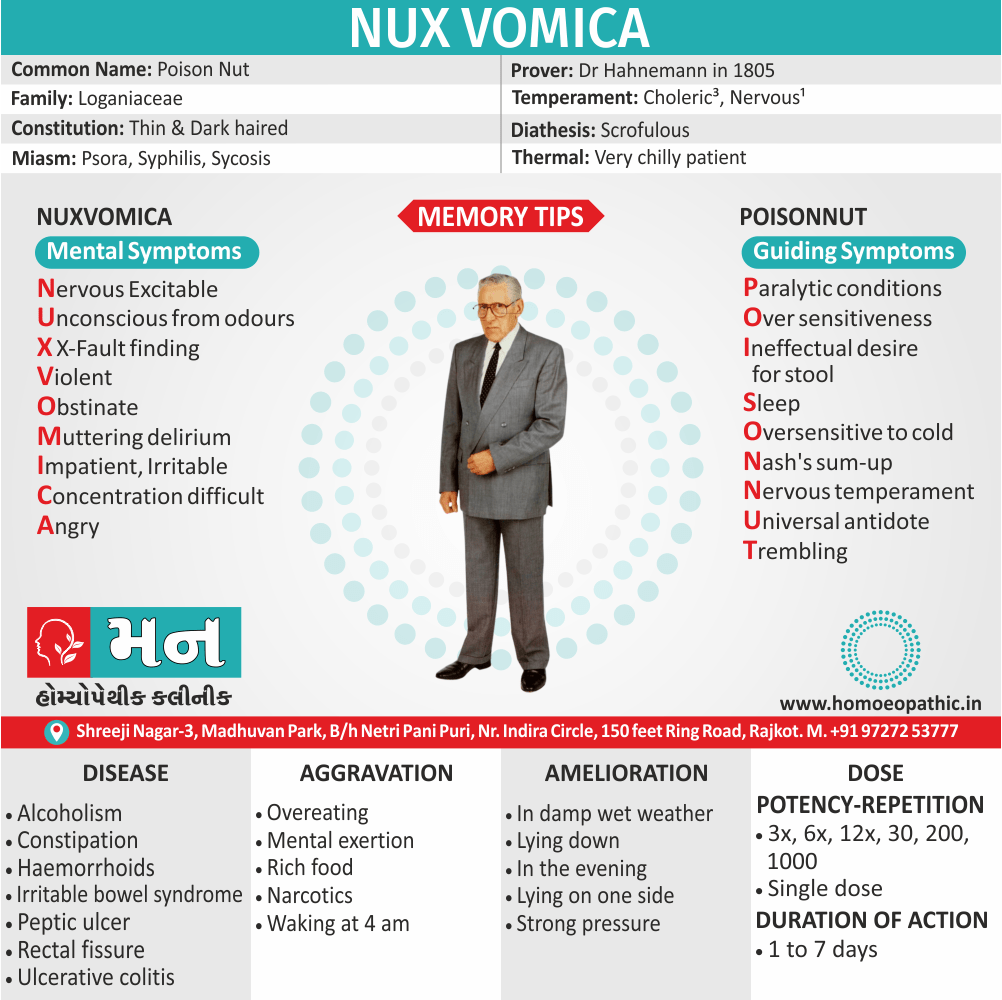
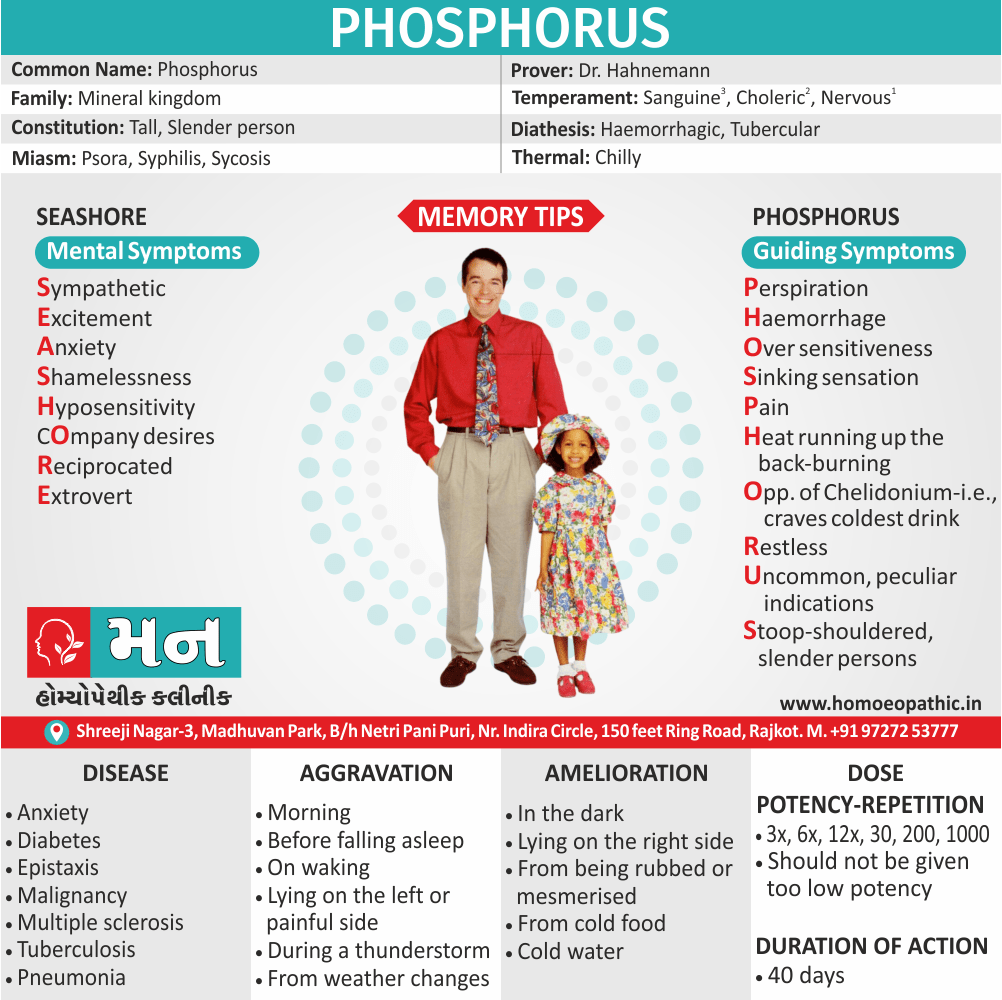
For instance; agaricus, anacardium, hyoscyamus, nux vomica, lilium tig, phosphorus.
8. Dementia after epileptic attack–
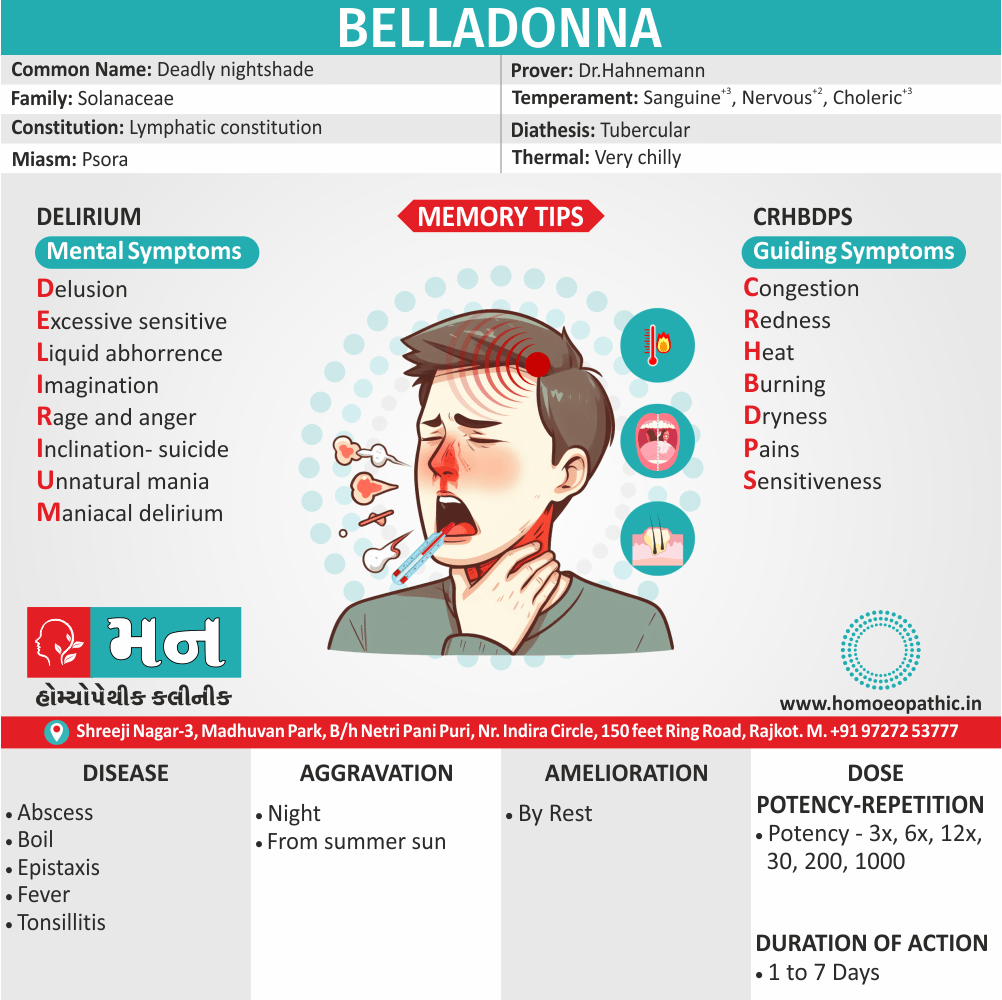
e.g. aconite, belladonna, silica.
9. Dementia due to depression–
tarentula.
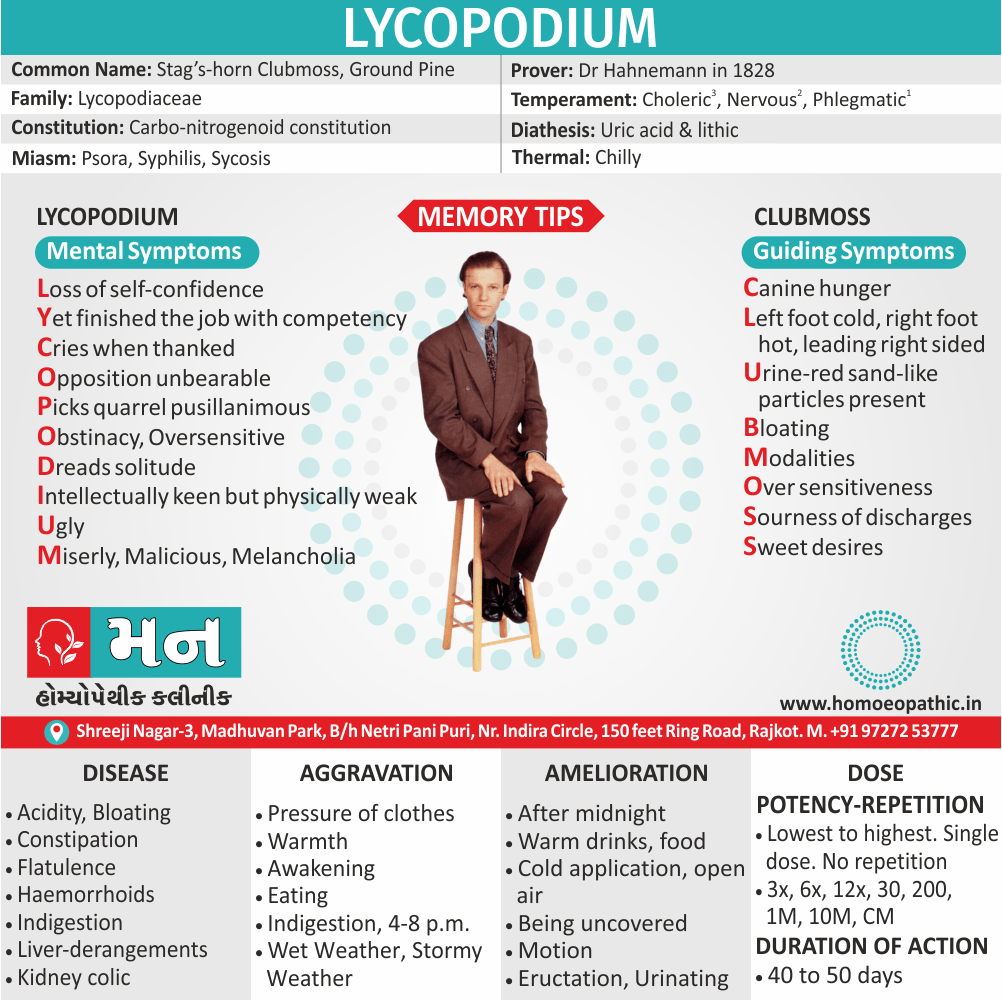
10. Senile dementia (in other words; Alzheimer’s disease)–
agnus castus, anacardium, conium, crotalus hor, lycopodium.
11. Specific remedies, which can be given every 12 hours for up to 3 doses for dementia:
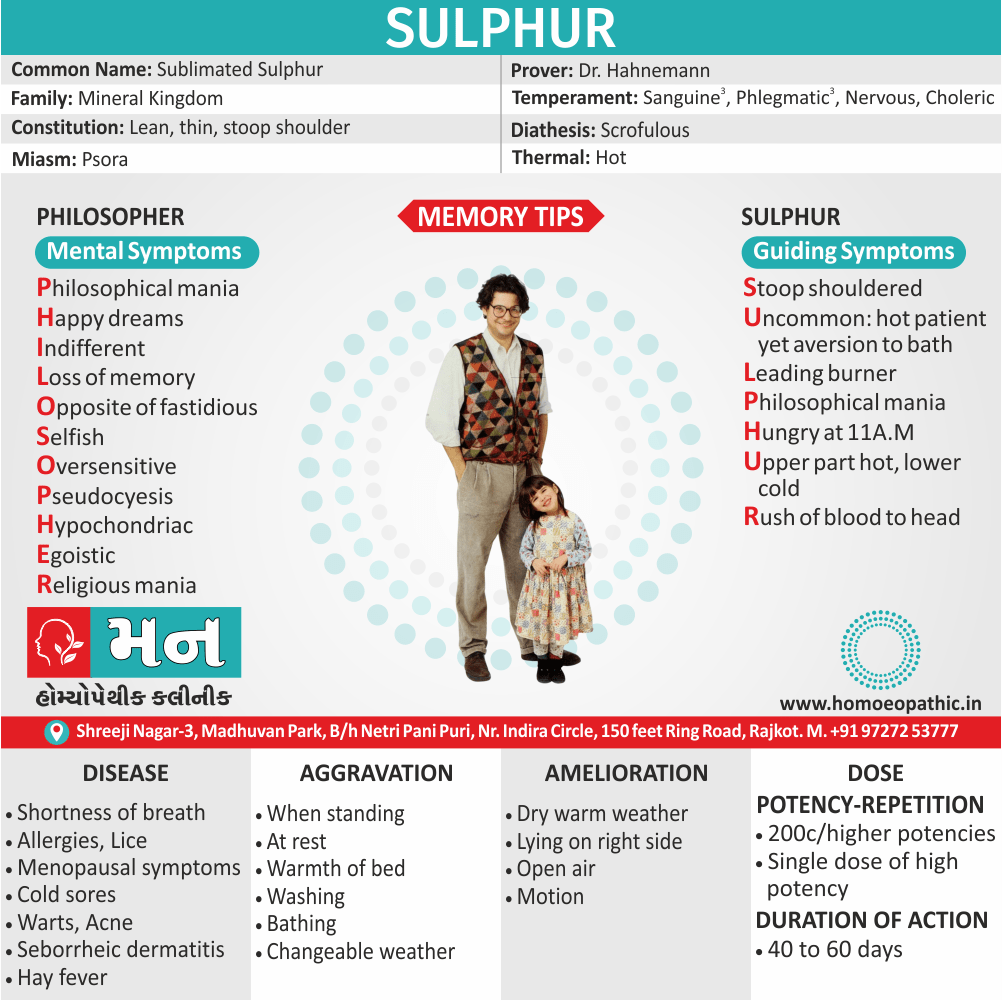
(a) Person once intellectually sharp and ambitious, now thin and withered, lacking in self-confidence, afraid of being alone, always using wrong words Lycopodium 30c.
(b) Degenerative changes in blood vessels, enlarged prostate gland, weakness and tiredness, problems exacerbated by cold Batuta 30c.
(c) Partial paralysis, blood vessels supplying brain affected by arteriosclerosis Auruti iod 30c.
(d) Atherosclerosis, craving for salt, person highly strung and very apprehensive Phosphorus 30c. [3]
Diet & Regimen of Dementia
- Eat green leafy vegetables.
- Limit foods with high saturated fat and cholesterol.
- Take beans and nuts in your diet.
- Eat a well-balanced diet daily.
- Cut down on refined sugar.
Frequently Asked Questions
What is Dementia?
Dementia is a generalized decline of intellect, memory, and personality, without impairment of consciousness, leading to functional impairment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Dementia?
- Agaricus
- Anacardium
- Hyoscyamus
- Nux vomica
- Lilium tig
- Phosphorus
- Aconite
- Belladonna
- Silica
- Tarentula
What are the symptoms of Dementia?
- Poor memory
- Impaired attention
- Aphasia, agnosia, also apraxia
- Disorientation
- ‘Personality change’
- Odd also disorganized
- Restless, wandering
- Self-neglect
- Social withdrawal Mood
- Anxiety, Depression
- Slow
- Delusions, Illusions, Hallucinations
- Impaired
What causes Dementia?
- Parenchymatous brain disease
- Vascular dementia
- Toxic dementias
- Metabolic dementias
- Traumatic dementias
- Thyroid, parathyroid
- Deficiency Dementias
- Neoplastic dementias
Reference
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 26.
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 3.
- Homeopathy in Treatment Of Psychological Disorders by Shilpa Harwani / Ch 17.
- Dementia Risk Factors | Stanford Health Care
- The pathophysiology of dementia – PubMed (nih.gov)
- Dementia physical examination,Differential diagnosis- wikidoc
- How to Help Prevent Dementia (healthline.com)
Overview
Epidemiology
Causes
Risk Factors
Types
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Dont’s
Terminology
References
FAQ
Also Search As
Overview
It is a clinical syndrome, rather than a diagnosis in itself, which may cause by a variety of pathologies. Dementia is an acquired disorder, as distinct from learning disability in which impairments are present from birth, although the onset may be at any age.
In either middle-aged or older person any social lapse that is out of character should always suggest dementia. [1]
Onset: Insidious
Course: Protracted, although may be reversible in some cases. [2]
Epidemiology
Indian epidemiology then other
Causes
Irreversible causes:
Parenchymatous brain disease i.e.:
Alzheimer’s disease, Pick’s disease, Parkinson’s disease, Huntington’s chorea, Lewy body dementia, Steel Richardson syndrome ( in other words, Progressive Supranuclear Palsy).
Vascular dementia i.e.:
Multi-infarct dementia, subcortical vascular dementia ( in other word, Binswanger’s disease).
Toxic dementias i.e.:
Bromide intoxication, drugs, heavy metals, alcohol, carbon monoxide, analgesics, anticonvulsants, benzodiazepines, also psychotropic drugs.
Metabolic dementias i.e.:
Chronic hepatic or uraemic encephalopathy, dialysis dementia, Wilson’s disease.
Traumatic dementias i.e.:
Chronic subdural haematoma, head injury.
Potentially reversible causes:
Endocrine causes i.e.:
Thyroid, parathyroid, pituitary, also adrenal dysfunction.
Deficiency Dementias i.e.:
Pernicious anaemia, pellagra, folic acid deficiency, also thiamine deficiency.
Neoplastic dementias i.e.:
Neoplasms and other intracranial space-occupying lesions.
Hydrocephalic dementia i.e.:
Normal pressure hydrocephalus. [2]
Risk Factors
Risk factors are things that make you more likely to develop a disease in the first place.
Risk factor of Dementia
Age. – The risk of Alzheimer’s disease, vascular dementia, and several other dementias goes up significantly with advancing age.
Genetics/family history- Researchers have discovered a number of genes that increase the risk of developing Alzheimer’s disease. Although people with a family history of Alzheimer’s disease are generally considered to be at a heightened risk of developing the disease themselves, many people who have relatives with Alzheimer’s disease never develop the disease, and many without a family history of the disease do get it.
Smoking and alcohol use- Several recent studies have found that smoking significantly increases the risk of mental decline and dementia. People who smoke have a higher risk of atherosclerosis and other types of vascular disease, which may be the underlying causes for the increased dementia risk.
Atherosclerosis.- Atherosclerosis is the buildup of plaque – deposits of fatty substances, cholesterol, and other matter – in the inner lining of an artery.
Atherosclerosis is a significant risk factor for vascular dementia, because it interferes with the delivery of blood to the brain and can lead to stroke. Studies have also found a possible link between atherosclerosis and Alzheimer’s disease.
Cholesterol- High levels of low-density lipoprotein (LDL), the so-called "bad" form of cholesterol, appear to significantly increase a person’s risk of developing vascular dementia. Some research has also linked high cholesterol to an increased risk of Alzheimer’s disease.
Plasma homocysteine- Research has shown that a higher-than-average blood level of homocysteine, a type of amino acid, is a strong risk factor for the development of Alzheimer’s disease and vascular dementia.
Diabetes- Diabetes is a risk factor for both Alzheimer’s disease and vascular dementia. It is also a known risk factor for atherosclerosis and stroke, both of which contribute to vascular dementia.
Mild cognitive impairment- While not all people with mild cognitive impairment develop dementia, people with this condition do have a significantly increased risk of dementia compared to the rest of the population.(4)
Types
1.Alzheimer’s Dementia:
This is the commonest cause of dementia, seen in about 70% of all cases of dementia in USA. It is more commonly seen in women. Earlier, it was differentiated into two forms: a presenile form and a senile
form. Autopsy shows macroscopic changes such as enlarged cerebral ventricles, widened cerebral sulci and shrinkage of cerebral cortex.
Neurochemically, there is a marked decrease in brain choline acetyltransferase (in other words, CAT) with a similar decrease in brain acetylcholinesterase (AchE).
Treatment:
Cholinesterase Inhibitors:
- Rivastigmine(1.5 mg twice a day to 6 mg twice a day).
- Donepezil(5-10 mg/day).
- Galantamine (4 mg twice a day to 12 mg twice a day) have used in the recent past for treatment of moderate dementia with Alzheimer’s disease.
These elevate acetylcholine (Ach) concentrations in cerebral cortex by slowing the degradation of acetylcholine released by still intact cholinergic neurons in Alzheimer’s disease.
Memantine (5-20 mg/day), an N-methyl-D’Aspartate (NMDA) antagonist, is also available for the treatment of moderately severe to severe Alzheimer’s disease.
2. Multi-infarct Dementia:
Multi-infarct dementia is the second commonest cause of dementia, seen in 10-15% of all cases, though it is probably more common in India. Occurrence of multiple cerebral infarctions can lead to a progressive disruption of brain function, leading to dementia.
The most typical form of multi-infarct dementia is characterised by the following features:
1. An abrupt onset.
2. Acute exacerbations (due to repeated infarct ions).
3. Stepwise clinical deterioration (especially, step-ladder pattern).
4. Fluctuating course.
5. Presence of hypertension (most commonly) or any other significant cardiovascular disease.
6. History of previous stroke or transient ischemic attacks (in other words, TIAs).
Diagnosis: Emotional lability is common. EEG (specifically, showing focal area of slowing) and brain imaging (either CT scan or MRI scan of brain showing multiple infarcts) help in diagnosis.
3. Hypothyroid Dementia:
This has been considered one of the most important treatable also reversible causes of dementia, second only to toxic dementias.
Although it accounts for less than 1% of dementias, hypothyroidism should be suspected in every patient of dementia.
All in all, Prompt treatment can reverse the dementing process and can lead to complete recovery if the treatment is start within two years of the onset of dementia.
4. AIDS Dementia Complex:
About 50-70% of patients suffering from AIDS exhibit a triad of cognitive, behavioural and motoric deficits of subcortical dementia type and this is known as the AIDS-dementia complex (in other words, ADC).
As the AIDS virus (a lentivirus, a type of retrovirus) is highly neurotropic and the virus crosses the blood-brain barrier early in the course of the disease cognitive impairment is nearly ubiquitous in AIDS.
Diagnosis: The diagnosis is established by ELISA (enzyme linked immunosorbent assay) showing anti-HIV antibodies, and the Western Blot test (blotting of antibody specificities to HIV-specific proteins).
A Cranial CT scan can show cortical atrophy 1-4 months before the onset of clinical dementia while MRI scan is helpful in detecting the white matter lesions.
5. Lewy Body Dementia:
Lewy body dementia is now believe to be the second most common cause of the degenerative dementias, accounting for about 4% of all dementias.
Typically, the clinical features of Lewy body dementia include:
i. Fluctuating cognitive impairment over weeks or months, with involvement of memory and higher cortical functions (such as language, visuo-spatial ability, praxis and reasoning). Lucid intervals can be present in between fl uctuations.
ii. Recurrent and detailed visual hallucinations.
iii. Spontaneous extrapyramidal or parkinsonian symptoms such as rigidity and tremors.
iv. Neuroleptic sensitivity syndrome, characterised by a marked sensitivity to the effects of typical doses of antipsychotic drugs (resulting in severe extrapyramidal side-effects with use of antipsychotics).
Other clinical features:
It may include repeated falls, autonomic dysfunction (e.g. orthostatic hypotension), urinary incontinence, delusions and depressive features.
Although Lewy bodies (intracytoplasmic inclusion bodies) are also present in Parkinson’s disease, the occurrence of Lewy bodies in Lewy body dementia is more widespread. Antipsychotic medication should be avoided (or used with extreme caution and in low doses) in patients with Lewy body dementia.
Diagnosis: A PET (Positron Emission Tomography) or SPECT (Single Photon Emission Computerised Tomography) scan of brain may show low dopamine transporter uptake in basal ganglia. [2]
Pathophysiology
Pathophysiology of Dementia
- Dementia is a symptom of a variety of specific structural brain diseases as well as several system degenerations.
- Alzheimer’s disease presently is the commonest cause in the developed world, causing a cortical-subcortical degeneration of ascending cholinergic neurons and large pyramidal cells in the cerebral cortex.
- Clinically, the disease reflects predominantly deterioration of function in the association cortex.
- Pharmacologically and pathologically, abnormalities are more diffuse and extend into sensorimotor cortical areas as well. (6)
Clinical Features
Tab Content
Sign & Symptoms
Cognition such as:
- Poor memory
- Impaired attention
- Aphasia, agnosia, and apraxia
- Disorientation
- ‘Personality change’
Behaviour such as:
- Odd and disorganized
- Restless, wandering
- Self-neglect
- Disinhibition
- Social withdrawal Mood
Anxiety i.e.:
- Anxiety
- Depression
Thinking i.e.:
- Slow, impoverished
- Delusions
Perception such as:
- Illusions
- Hallucinations
Insight such as:
- Impaired. [1]
Clinical Examination
Clinical examination of Dementia
A thorough general physical examination followed by focused focal neurologic deficits examination that may be consistent with prior strokes, parkinsonism (rigidity and/or tremors), gait abnormalities or slowing, and eye movements should be preferably done. Some patients with Alzheimer disease (AD) generally have no motor or sensory deficits at presentation.
The final diagnosis of dementia is made on the basis of the clinical picture, increasingly with neuroimaging results for backup. For research purposes, the diagnosis depends on both a clinical diagnosis and a pathological diagnosis (i.e., based on the examination of brain tissue, usually from autopsy).
Proper differential diagnosis between the types of dementia (see below) will require, at the least, referral to a specialist, e.g. a geriatric internist, geriatric psychiatrist, neurologist, neuropsychologist or gero psychologist. However, there are some brief (5-15 minutes) tests that have good reliability and can be used in the office or other setting to evaluate cognitive status. Examples of such tests include the abbreviated mental test score (AMTS), the mini mental state examination (MMSE), Modified Mini-Mental State Examination (3MS), the Cognitive Abilities Screening Instrument (CASI and the clock drawing test.
An AMTS score of less than six (out of a possible score of ten) and an MMSE score under 24 (out of a possible score of 30) suggests a need for further evaluation. Scores must be interpreted in the context of the person’s educational and other background, and the particular circumstances (for example, a person in great pain will not be expected to do well on many tests of mental ability). (6)
Diagnosis
According to ICD-10, the following features are required for diagnosis:
- Evidence of;
Decline in both memory and thinking, sufficient enough to impair personal activities of daily living
Memory impairment (typically affecting registration, storage, and retrieval of new information though previously learned material may also be lost particularly in later stages.
Impaired thinking, presence of clear consciousness (consciousness can be impaired if delirium is also present), and a duration of at least 6 months. [2]
- The Mini Mental State Examination (MMSE) is used widely in assessment; it combines standard questions with tests of spatial ability, and has high sensitivity and specificity. [2]
Differential Diagnosis
Differential diagnosis of dementia
- Delirium
- Depression
- Amnestic disorders
- Aphasias
- Vitamin B12 deficiency
- Vitamin B6 deficiency
- Thiamine deficiency
- Parkinson’s disease
- Marijuana abuse
- Vascular dementia
- AIDS. (6)
Complications
Complications are what happen after you have a disease. They are the negative consequences of the disease process.
Investigations
Investigation of Dementia
Laboratory Investigations:
- Basic Haematology
- Biochemistry
- Liver function
- Thyroid function
- Vitamin B12
- Folate
- Thiamine
- Calcium
- Glucose.
Imaging:
- A CT or MRI brain scan may be needed, as they are valuable in the diagnosis of both focal and diffuse cerebral pathology. [1]
- Focused history, mental status examination, and functional assessment.
- Measurement of the protein 14-3-3 in cerebrospinal fluid (CSF)
- CSF concentrations of tau protein and beta-amyloid peptide 42
Treatment
General measures:
- Treat any physical disorders
- Psychoeducation of patient, family, also carers
- Promote and maintain independence with a written care plan
- besides this, Provide training courses and support groups for carers
- Respite care
- Lastly, Palliative care input
Psychological:
- Structured group cognitive stimulation programme
- For agitation: For example; aromatherapy, dance/music therapy, animal therapy
- Psychological support for carers
Pharmacological:
- Acetylcholinesterase inhibitors: (e.g. Donepezil, Galantamine, Rivastigmine) increase the concentration of and duration of action of acetylcholine in the central nervous system. Additionally, There is evidence that in moderately severe Alzheimer’s disease, these drugs improve cognitive function and behaviour for up to a year. All in all, these drugs should only be prescribed by specialists, and should be stopped after 6 months if there is no clinical benefit.
- Memantine: It is a glutamine NMDA receptor antagonist which improves cognition, mood, and behaviour in moderate to severe Alzheimer’s.
- For agitation such as:
Antipsychotics : Antipsychotics should generally be avoided whenever possible and only have a role in patients with severely distressing symptoms or agitation causing risk to self or others.
They should be avoided in those with mild to moderate dementia, as there is a slight increase in the risk of cerebrovascular events.
The recommended drugs are haloperidol also olanzapine. A few patients need long-term oral antipsychotics to manage their behaviour at home.
Benzodiazepines: Benzodiazepines should be avoided wherever possible, especially during the day.
Intramuscular lorazepam is a suitable alternative to an antipsychotic for extreme agitation, also should be tried if antipsychotics do not relieve the symptoms.
- For depression: e.g. antidepressants. [1]
Prevention
Prevention of Dementia
Exercise
- Regular physical activity can help reduce the risk of dementia
Eat well
- A diet that’s good for the heart is good for the brain and overall health. A healthy diet may reduce your risk of conditions that can lead to dementia. According to the World Health Organization (WHO), a balanced diet consists of:
- fruit and vegetables
- lentils and beans
- grains, tubers, or roots
- eggs, milk, fish, lean meat
Things to avoid or keep to a minimum are:
- saturated fats
- animal fats
- sugars
- salt
Your diet should center around nutrient-rich, whole foods. Avoid high calorie, processed foods that provide little to no nutritional value.
Don’t smoke
- Research Trusted Source shows that smoking can increase the risk of dementia, especially if you’re 65 years old or more. Smoking affects blood circulation all around your body, including the blood vessels in your brain.
Keep your mind active
An active mind may help lower the risk of dementia, so keep challenging yourself. Some examples would be:
- study something new, like a new language
- do puzzles and play games
- read challenging books
- learn to read music, take up an instrument, or start writing
- stay socially engaged: keep in touch with others or join group activities
- volunteer
Manage overall health
Staying in good shape can help lower risk of dementia, so get a yearly physical. See your doctor if you have symptoms of:
- depression
- hearing loss
- sleep problems
Manage existing health conditions such as:
- diabetes
- heart disease
- high blood pressure
- high cholesterol (7)
Homeopathic Treatment
Homeopathic Treatment of Dementia
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Dementia
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
. Anacardium Orientale – A Top Homeopathic Medicine for Dementia
Anacardium Orientale is among the best homeopathic remedies for dementia. Patients needing Anacardium Orientale have impaired memory and marked forgetfulness. The patient suddenly forgets the names of those around and also forgets things he has recently seen. Forgetfulness makes the person low spirited. There is also a marked absent mindedness and a deficiency of ideas. Homeopathy also uses Anacardium Orientale for the treatment of Alzheimer’s.
2. Baryta Carb – A Homeopathic Remedy for Senile Dementia
Baryta Carb is an excellent homeopathic remedy for senile dementia. In such cases, there is progressing mental weakness. There is forgetfulness while speaking and the mind seems clouded. The patient tends to forget the words that he is about to speak. There is a loss of memory, and when the patient tries to recollect past events, he is unable to do so. Baryta Carb works well for the treatment of dementia in the elderly who may have lost mental function after a stroke.
3. Cannabis Indica – Homeopathic Medicine for Dementia with Difficulty in Communication
Cannabis Indica is one of the best homeopathic remedies for dementia in cases where there is difficulty in communication. Cannabis Indica is helpful where a person becomes extremely forgetful while communicating. He forgets the last words spoken by him as well as what he is about to say. He begins to speak a sentence and then suddenly loses the thread of conversation. While writing too, the patient forgets what he intends to write. The mind is foggy, and there is an inability to recall past events. Difficulty in focusing is also experienced.
4. Medorrhinum – Homeopathic Medicine for Dementia Where the Patient Forgets Names and Words
Medorrhinum is a suitable homeopathic medicine for dementia where the person forgets names and words. The main symptom that points to the use of Medorrhinum is forgetting the names of friends and familiar people. The patient may not even remember their own name. There is also forgetfulness while writing, both regarding the words that are to be written as well as their spelling. While speaking, the person may forget the appropriate words. During a conversation, the patient may forget what he was asked; and the question has to be repeated. Along with the above symptoms, there are severe mood changes as well. Happiness alternates with sadness. There is also marked irritability over small things.
5. Graphites Naturalis – Homeopathic Medicine for Dementia when Indifference Accompanies Memory Loss
Graphites Naturalis is one of the best homeopathic remedies for dementia in cases where indifference accompanies memory loss. The person forgets recent events but remembers past events that occurred at a young age. There is indifference to everything and everybody. Along with this, the patient may be obstinate and moody. Dullness and anxiety, mostly in the mornings, also occur.
6. Kali Phos – A Useful Homeopathic Medicine for Dementia when Prostration Accompanies Memory Loss
Kali Phos is an effective homeopathic medicine for dementia. The main symptom pointing towards the use of Kali Phos is memory loss accompanied by tiredness. There is exhaustion on both mental and physical levels. In such cases, the patient doesn’t recognize his surroundings and is not inclined to speak with others. Sometimes, gloominess, depression, nervousness, and anxiety are also present.
7. Dementia, due to schizophrenia–
For instance; agaricus, anacardium, hyoscyamus, nux vomica, lilium tig, phosphorus.
8. Dementia after epileptic attack–
e.g. aconite, belladonna, silica.
9. Dementia due to depression–
tarentula.
10. Senile dementia (in other words; Alzheimer’s disease)–
agnus castus, anacardium, conium, crotalus hor, lycopodium.
11. Specific remedies, which can be given every 12 hours for up to 3 doses for dementia:
(a) Person once intellectually sharp and ambitious, now thin and withered, lacking in self-confidence, afraid of being alone, always using wrong words Lycopodium 30c.
(b) Degenerative changes in blood vessels, enlarged prostate gland, weakness and tiredness, problems exacerbated by cold Batuta 30c.
(c) Partial paralysis, blood vessels supplying brain affected by arteriosclerosis Auruti iod 30c.
(d) Atherosclerosis, craving for salt, person highly strung and very apprehensive Phosphorus 30c. [3]
Diet & Regimen
Diet & Regimen of Dementia
- Eat green leafy vegetables.
- Limit foods with high saturated fat and cholesterol.
- Take beans and nuts in your diet.
- Eat a well-balanced diet daily.
- Cut down on refined sugar.
Do’s and Dont’s
Tab Content
Terminology
Tab Content
References
Reference
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 26.
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 3.
- Homeopathy in Treatment Of Psychological Disorders by Shilpa Harwani / Ch 17.
- Dementia Risk Factors | Stanford Health Care
- The pathophysiology of dementia – PubMed (nih.gov)
- Dementia physical examination,Differential diagnosis- wikidoc
- How to Help Prevent Dementia (healthline.com)
FAQ
Frequently Asked Questions
What is Dementia?
Dementia is a generalized decline of intellect, memory, and personality, without impairment of consciousness, leading to functional impairment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Dementia?
- Agaricus
- Anacardium
- Hyoscyamus
- Nux vomica
- Lilium tig
- Phosphorus
- Aconite
- Belladonna
- Silica
- Tarentula
What are the symptoms of Dementia?
- Poor memory
- Impaired attention
- Aphasia, agnosia, also apraxia
- Disorientation
- ‘Personality change’
- Odd also disorganized
- Restless, wandering
- Self-neglect
- Social withdrawal Mood
- Anxiety, Depression
- Slow
- Delusions, Illusions, Hallucinations
- Impaired
What causes Dementia?
- Parenchymatous brain disease
- Vascular dementia
- Toxic dementias
- Metabolic dementias
- Traumatic dementias
- Thyroid, parathyroid
- Deficiency Dementias
- Neoplastic dementias
Also Search As
Frequently Asked Questions (FAQ)
XYZ
XXX
XYZ
XXX
XYZ
XXX
People found Homeopathic Clinic For XXXX by searching for
XXX
People found Homeopathic Doctors for XXXX by searching for
XXX
People found Homeopathic treatment for XXXX by searching for
XXX