Delirium:
Definition:
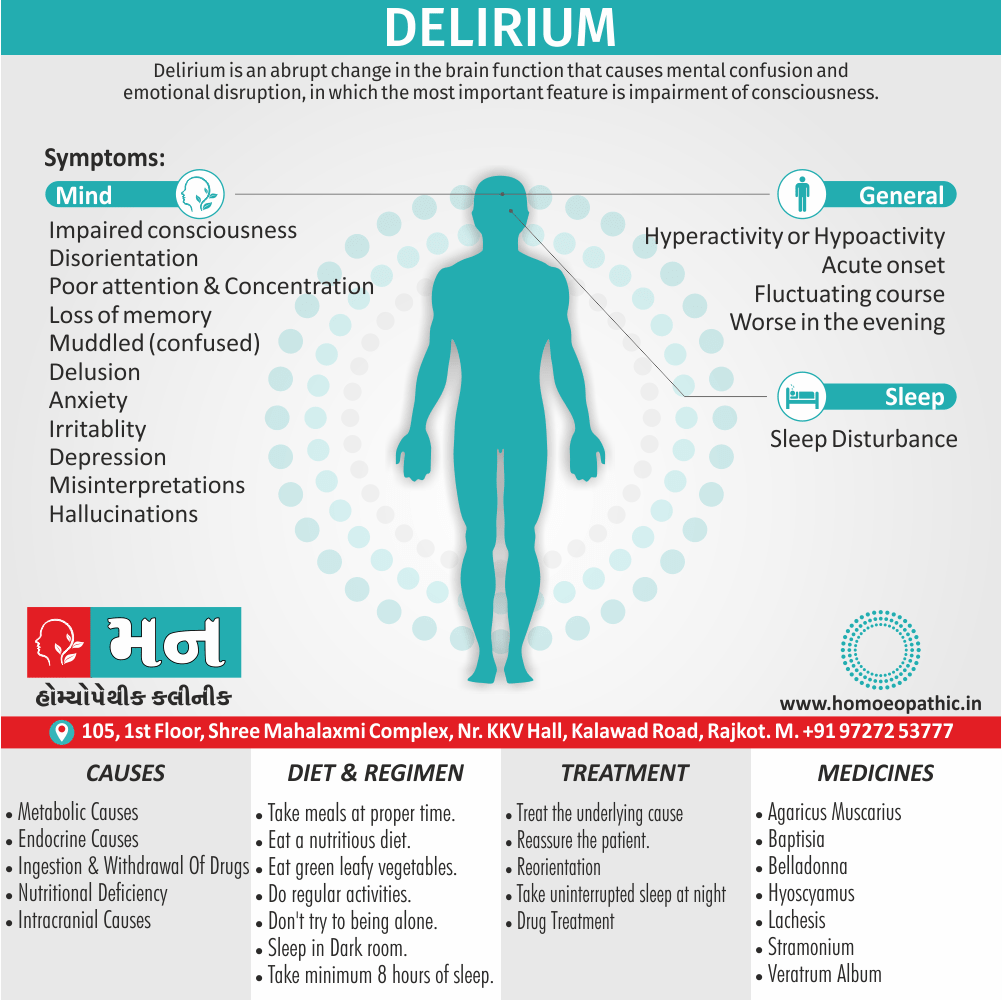
Delirium is the commonest organic mental disorder in clinical practice. [2]
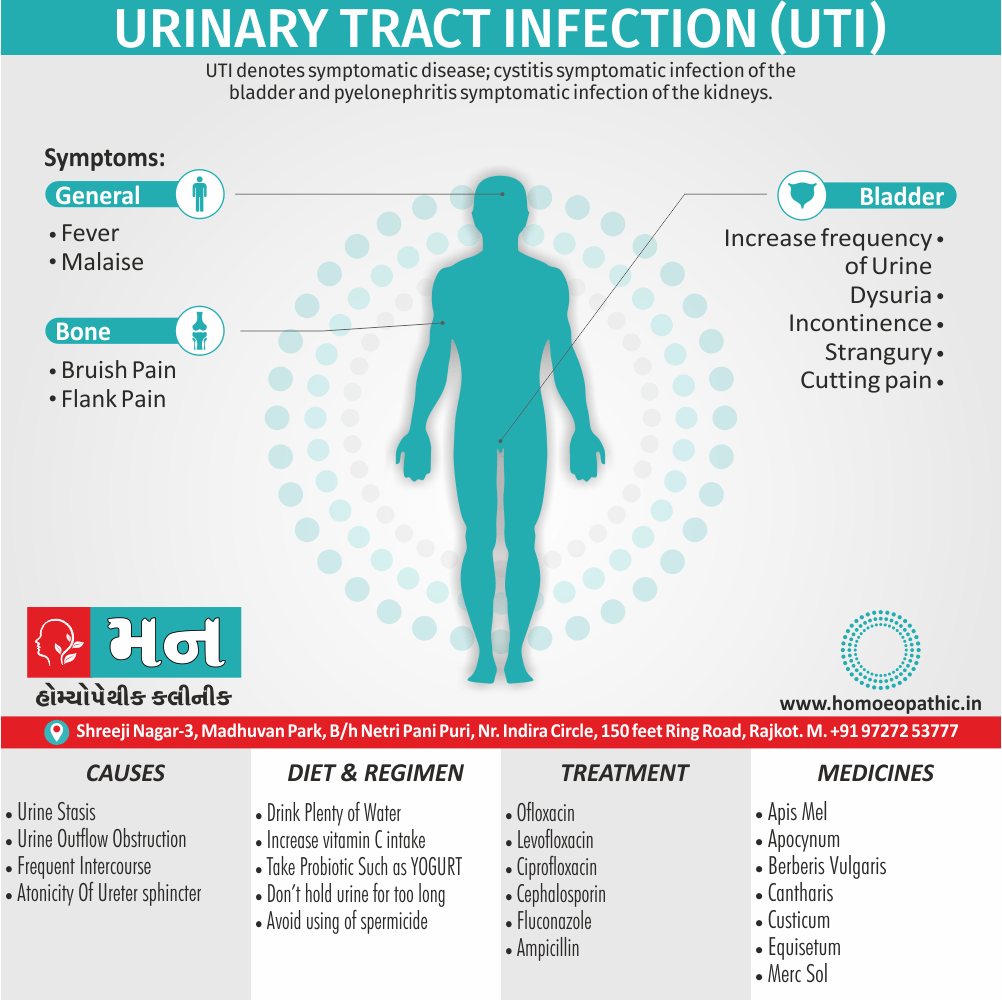
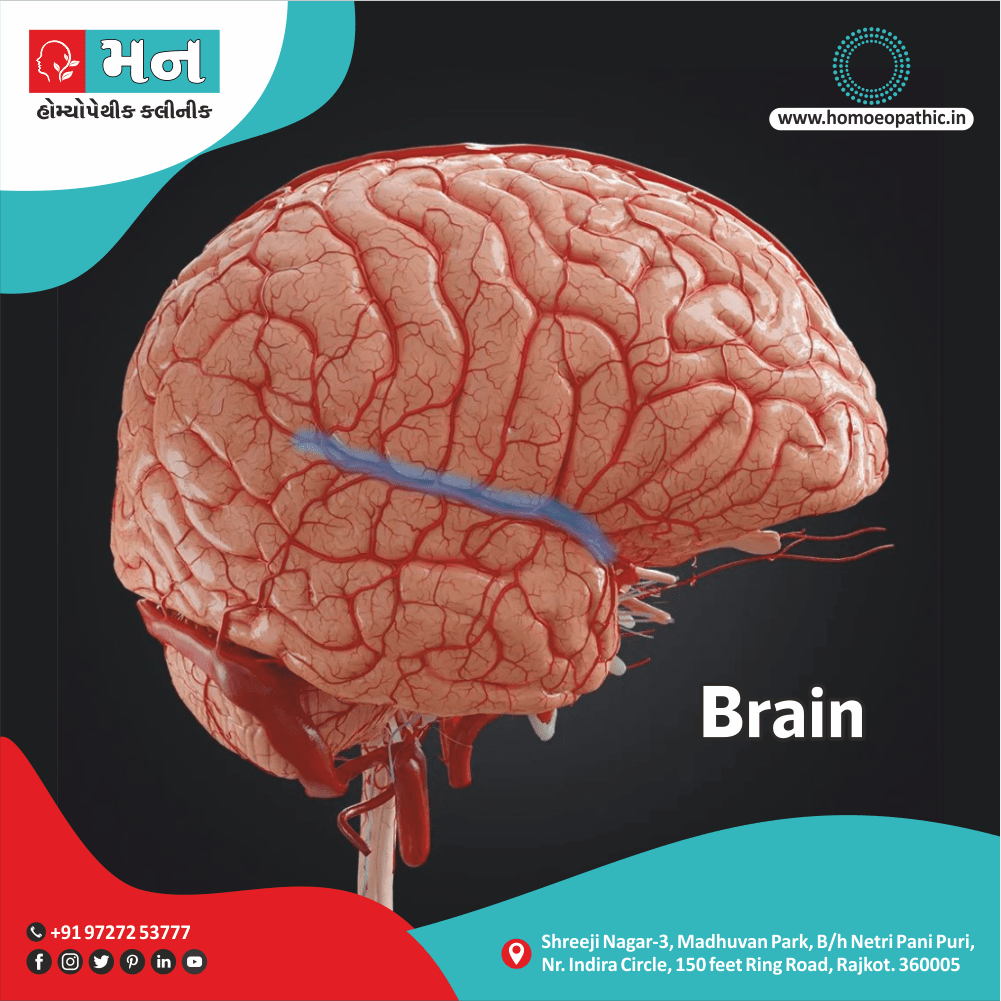
Delirium is an acute generalize impairment of brain function, in which the most important feature is impairment of consciousness. The disturbance of brain function is generalized, and the primary cause is often outside the brain; for example, sepsis due to a urinary tract infection. [1]
Causes of Delirium
Metabolic Causes:
i. Hypoxia, Carbon dioxide narcosis
ii. Hypoglycaemia
iii. Hepatic encephalopathy, Uremic encephalopathy
iv. Cardiac failure, Cardiac arrhythmias, Cardiac arrest
v. Water and electrolyte imbalance (e.g. Water, Na+, K+, Mg++, Ca++)
vi. Metabolic acidosis or alkalosis
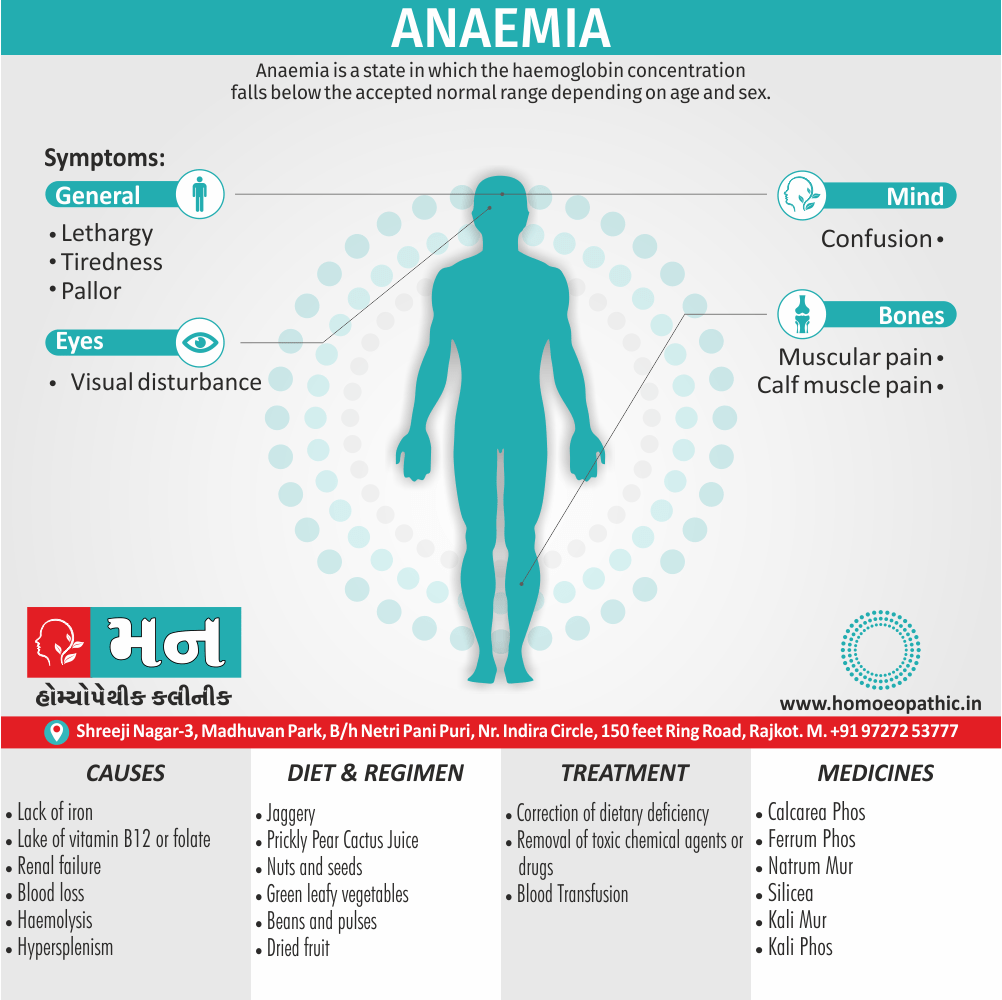
vii. Fever, Anaemia, Hypovolemic shock
viii. Carcinoid syndrome, Porphyria
viii. Carcinoid syndrome, Porphyria
Endocrine Causes:
i. Hypo- and Hyperpituitarism
ii. Hypo- and Hyperthyroidism
iii. Hypo- and Hyperparathyroidism
iv. Hypo- and Hyperadrenalism
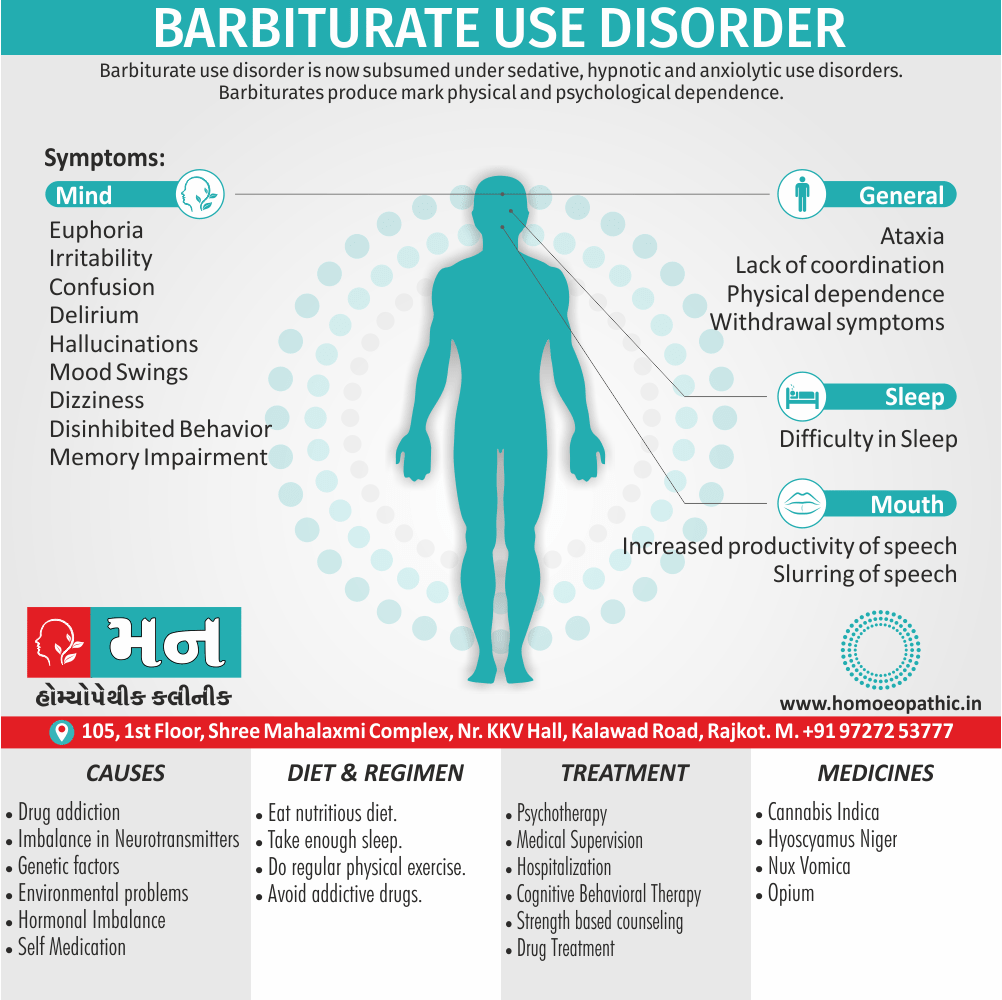
Drugs (Both ingestion and withdrawal can cause delirium) and Poisons:
i. Digitalis, Quinidine, Antihypertensives
ii. Alcohol, Sedatives, Hypnotics (especially barbiturates)
iii. Tricyclic antidepressants, Antipsychotics, Anticholinergics, Disulfiram
iv. Anticonvulsants,, L-dopa, Opiates
v. Salicylates, Steroids, Penicillin, Insulin
vi. Methyl alcohol, heavy metals, biocides
Nutritional Deficiencies:
i. Thiamine, Niacin, Pyridoxine, Folic acid, B12
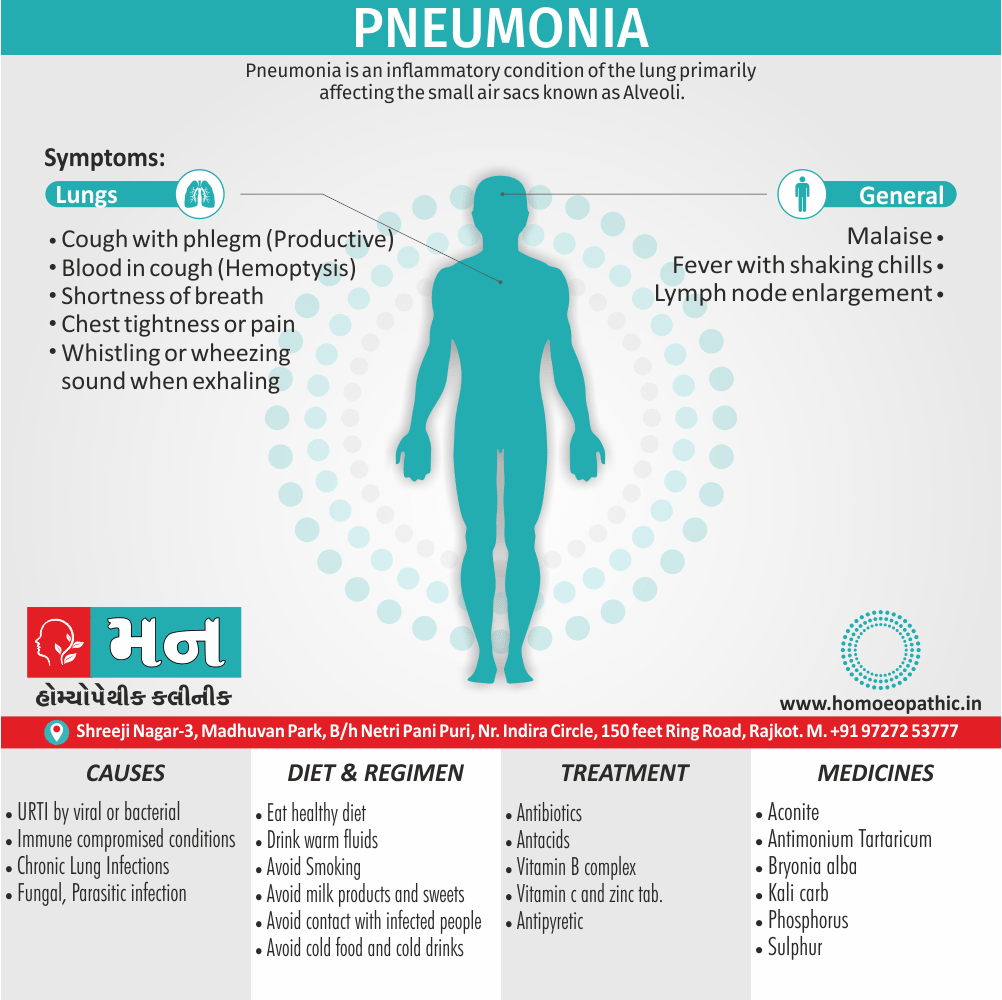
ii. Proteins Systemic Infections i. Acute and Chronic, e.g. Septicaemia, Pneumonia, Endocarditis
Intracranial Causes:
i. Epilepsy (i.e. postictal states)
ii. Head injury, Subarachnoid haemorrhage, Subdural haematoma
iii. Intracranial infections, e.g. Meningitis, Encephalitis, Cerebral malaria
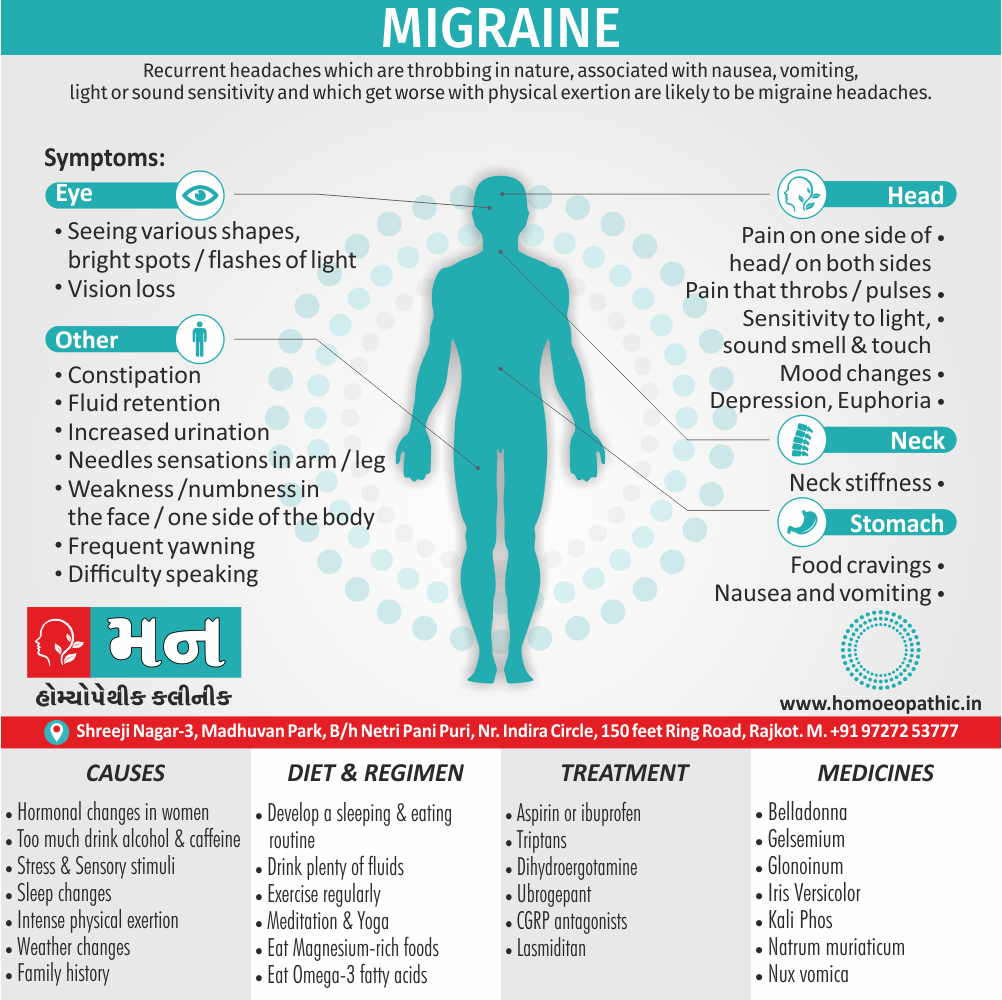
iv. Migraine
v. Stroke (especially; acute phase), Hypertensive encephalopathy
vi. Focal lesions, e.g. right parietal lesions (such as abscess, neoplasm)
Miscellaneous:
i. Postoperative states (including ICU delirium) ii. Sleep deprivation iii. Heat, Electricity, Radiation. [2]
Risk factors of Delirium
- Pre-existing dementia
- Severe medical Illness
- History of previous delirium
- Visual and hearing impairment
- Depression
- Abnormal sodium, potassium and glucose
- Polypharmacy
- Alcohol/ Benzodiazepine use
- Use of physical restraint
- Use of indwelling catheter
- Adding three or more medications
- Multiple bed moves
- Pain
- Surgery
- Anaesthesia and hypoxia
- Malnutrition and dehydration (4)
Pathophysiology of Delirium
-
The pathophysiology of delirium remains relatively unclear. In general, neuroimaging studies reveal disruptions in higher cortical functioning in multiple disparate areas of the brain, including the prefrontal cortex, subcortical structures, thalamus, basal ganglia, lingual gyri, and frontal, fusiform, and temporoparietal cortex.
-
Electroencephalographic (EEG) studies also show diffuse slowing of cortical activity.
-
Theories on the pathogenesis of delirium point to the role of neurotransmitters, inflammation, and chronic stress on the brain. For example, the role of cholinergic deficiency in inducing delirium is strengthened by the clear association of anticholinergic drug use with increased incidence. Studies in surgical patients have demonstrated a dysfunctional interaction between the cholinergic and immune systems in patients who developed postoperative delirium.
-
Dopaminergic excess is also believed to contribute. Evidence does not appear to support the use of antipsychotic medications (dopamine antagonists) for the prevention or treatment of delirium but is not entirely consistent.
-
Other neurotransmitters implicated in the pathophysiology of delirium include noradrenaline, serotonin, gamma-aminobutyric acid, glutamate, and melatonin.
-
Evidence also points to the role of cytokines such as interleukins 1 and 2 and TNF-alpha and interferon in contributing to delirium.
-
Finally, chronic hypercortisolism, as induced by chronic stress secondary to illness or trauma, may also contribute to delirium initiation.(6)
Types of delirium
Experts have identified three types:
- Hyperactive delirium- This may be the easiest type to recognize. People with this type may be restless and pace the room. They also may be anxious, have rapid mood swings or see things that aren’t there. People with this type often resist care.
- Hypoactive delirium- People with this type may be inactive or have reduced activity. They tend to be sluggish or drowsy. They might seem to be in a daze. They don’t interact with family or others.
- Mixed delirium- Symptoms involve both types of delirium. The person may quickly switch back and forth from being restless and sluggish. (5)
Sign & Symptoms of Delirium
- Impaired consciousness
- Disorientation
- Poor attention also concentration
- Loss of memory Behaviour
- Overactive
- Under active Thinking
- Muddled (in other words, confused)
- Ideas of reference
- Delusions Mood
- Anxious, irritable
- Depressed
- Perplexed
- Perception
- Misinterpretations
- Hallucinations, mainly visual
- Acute onset, fluctuating course, worse especially, in the evening
Impairment of consciousness is the most important symptom, and is seen as a deficit of attention, concentration, and awareness. Furthermore, Often the patient will not be able to follow or engage in a logical conversation. All in all, The features fluctuate in intensity and are often worse in the evening.
Disorientation: Uncertainty about the time, place, also identity of other people.
Behaviour may be either overactive, with noisiness and irritability, or underactive. Besides this, Sleep is often disturbed.
Thinking is slow and confused but the content is often complex. Ideas of reference also delusions are common.
Mood may anxious, perplex, either irritable or depress and is often labile.
Perception may distort with misinterpretations, illusions, and visual hallucinations. Additionally, Tactile and auditory hallucinations occur but are less frequent.
Memory : Generally, Disturbance of memory affects registration, retention, and recall, as well as new learning.
Insight is impaired. [1]
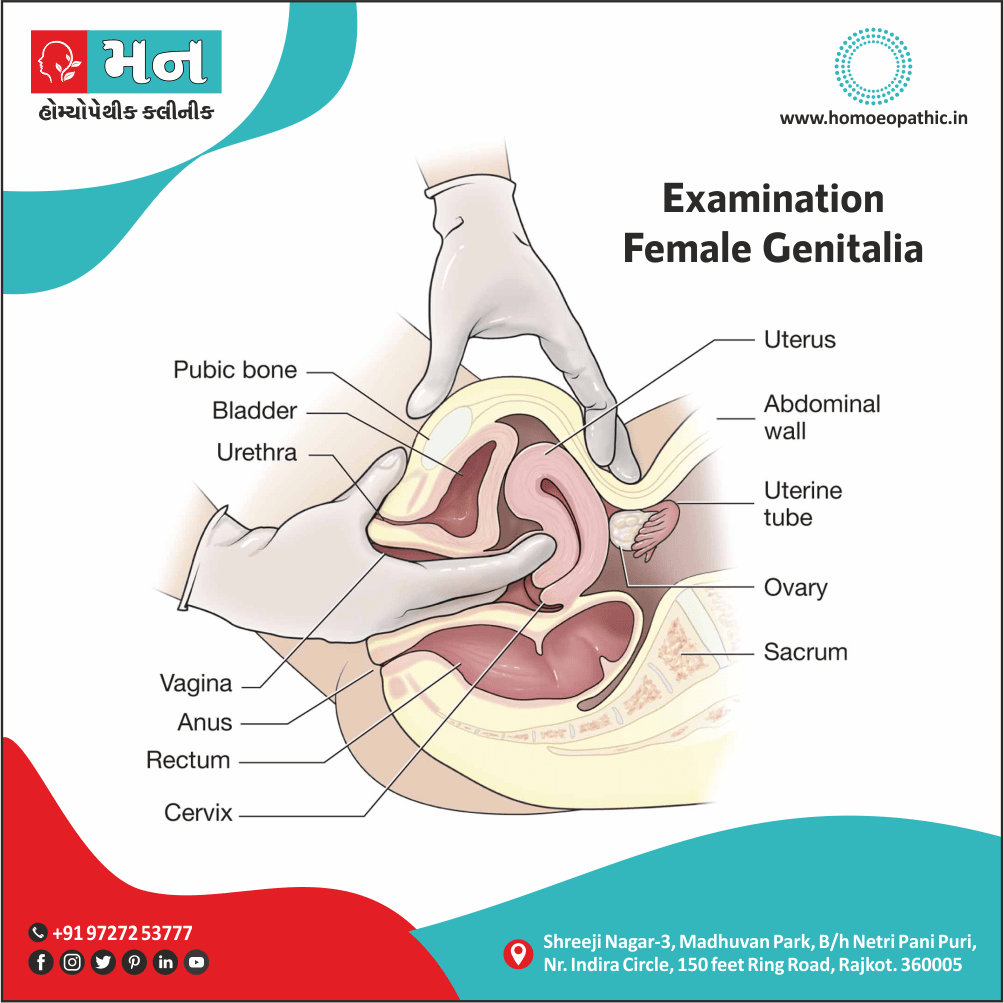
Clinical examination of Delirium
- Delirium symptom changes in severity during its course.
- It is essential to assess the patient multiple times, as it is easy to miss a diagnosis, also features like sundowning can be overlooked if the assessment is not done towards the end of the day.
General Examination
- Vital signs:
-
- Pulse: Increased pulse rate may be suggestive of heat failure, myocardial infarction or pulmonary pathology.
- Blood pressure: Malignant hypertension is an important cause of delirium, and blood pressure must be monitored if the patient is non compliant with antihypertensive medications.
- Low blood pressure may suggest heart failure.
- Appearance:
- Cherry red color indicates carbon monoxide poisoning,
- cyanosis may indicate respiratory or cardiac pathology.
- Jaundice may indicate hepatic or biliary pathology.
- Edema may be because of liver failure, cardiac failure, renal failure or malnutrition.
- Temperature:
- Fever may indicate underlying infection.
- Conscious level:
- Various levels of arousal can be seen in delirium, ranging from stupor to hyperarousal. If the patient appears to have a normal arousal level, attention deficit must be accessed which is very commonly seen in delirium.
- Cognitive function using a standardized screening tool, e.g. MoCA, Mini mental state examination or 4AT.
- Nutritional status: B12 and folate deficiencies can be assessed on physical examination.
- Hydration state: Dehydration as well as an overload of fluids, resulting in hypoxia can cause delirium.
- Infectious foci: Careful examination to rule out conditions such as meningitis, encephalitis, pulmonary consolidation etc.
- Evidence of intoxication or withdrawal for alcohol, and recreational drugs are an important part of delirium work up. Look for tremors, pupil size, needle tracks etc.
Systemic Examination
- Focused examination is necessary to find out underlying etiology.
-
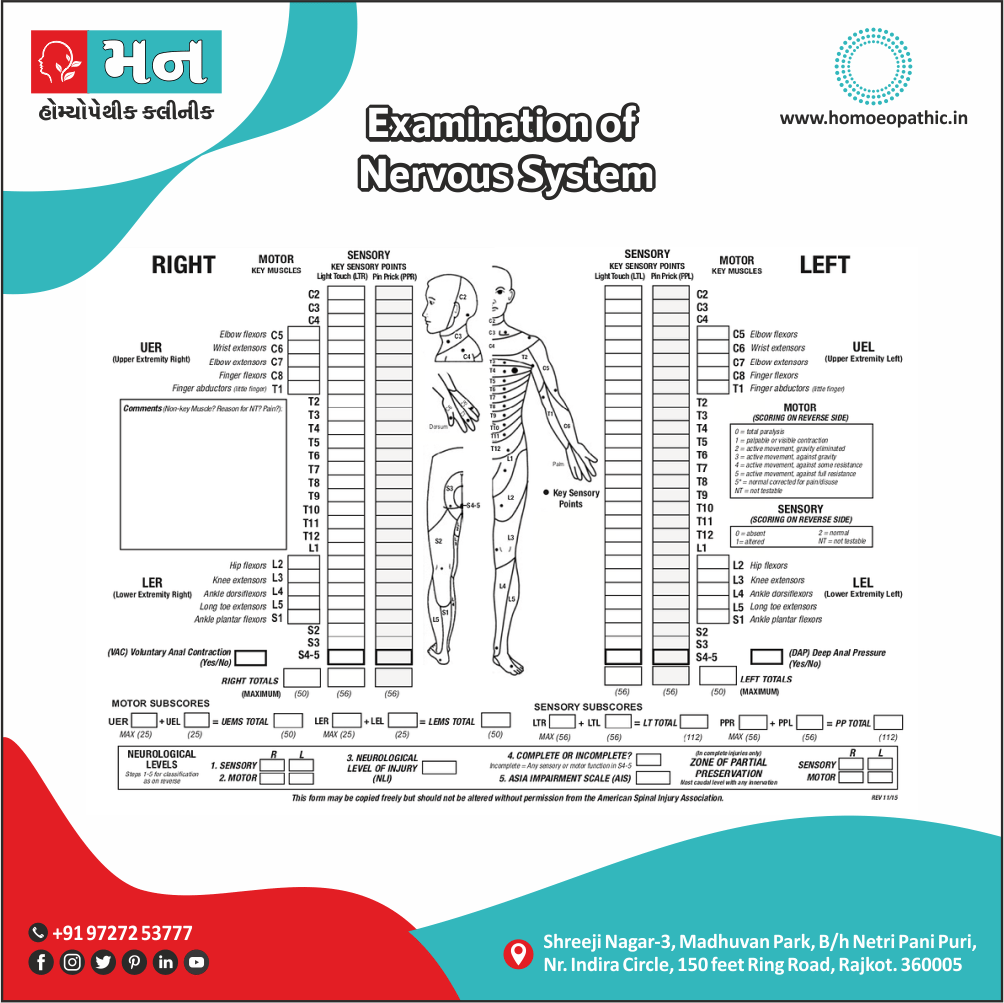
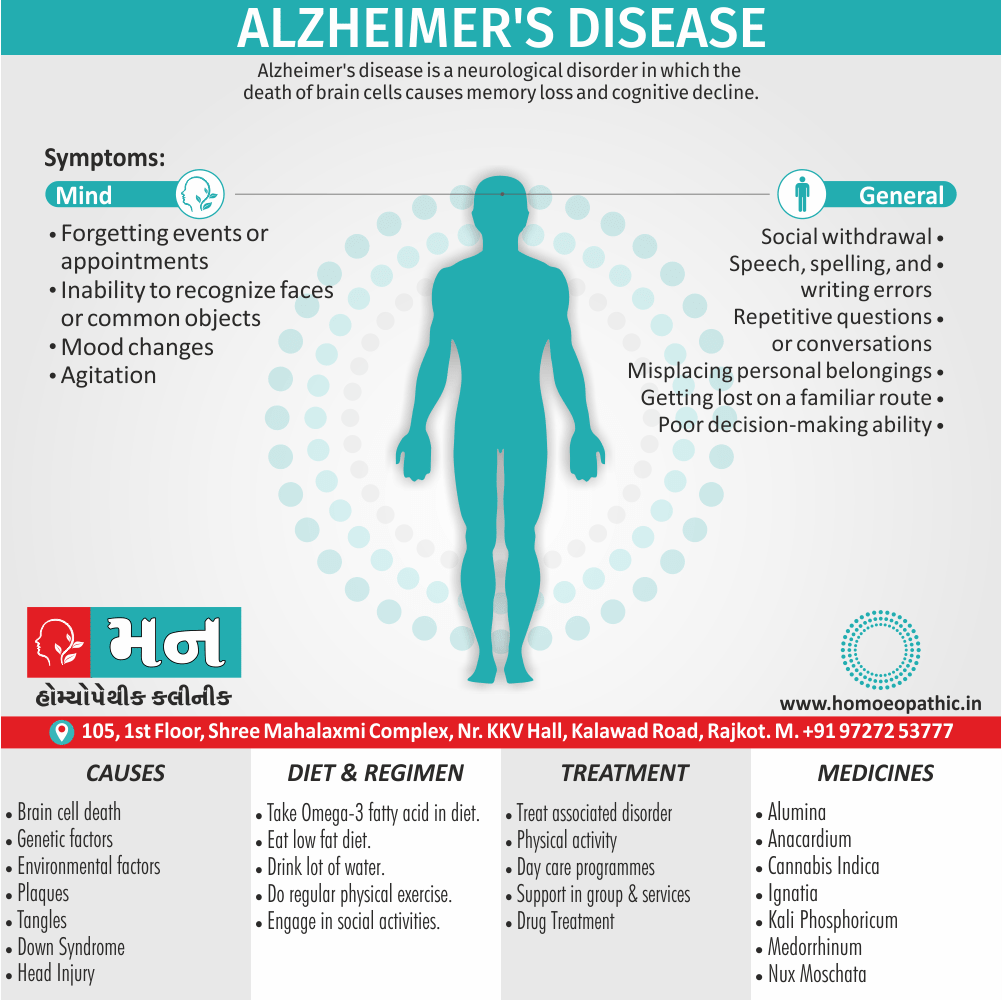
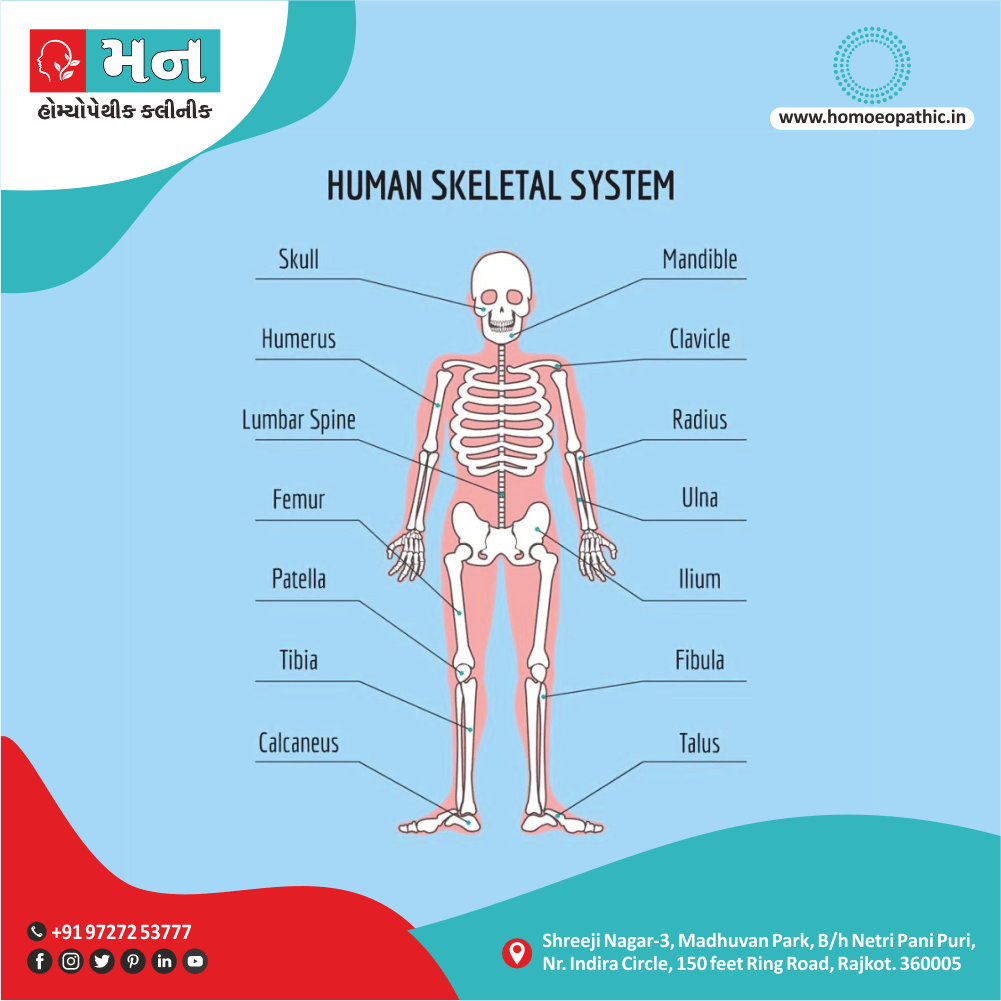
- Neurological examinations: Careful examination must be done to find out neurological causes of delirium, such as cerebrovascular diseases, neurodegenrative disorders such as parkinsonism, Alzheimer, and lewi body dementia.
- Many systemic diseases may show neurological manifestations: hepatic encephalopathy causes flapping tremor.
- Overdose and intoxication can also effect the central nervous system : opiates causes pinpoint pupils and respiratory depression.
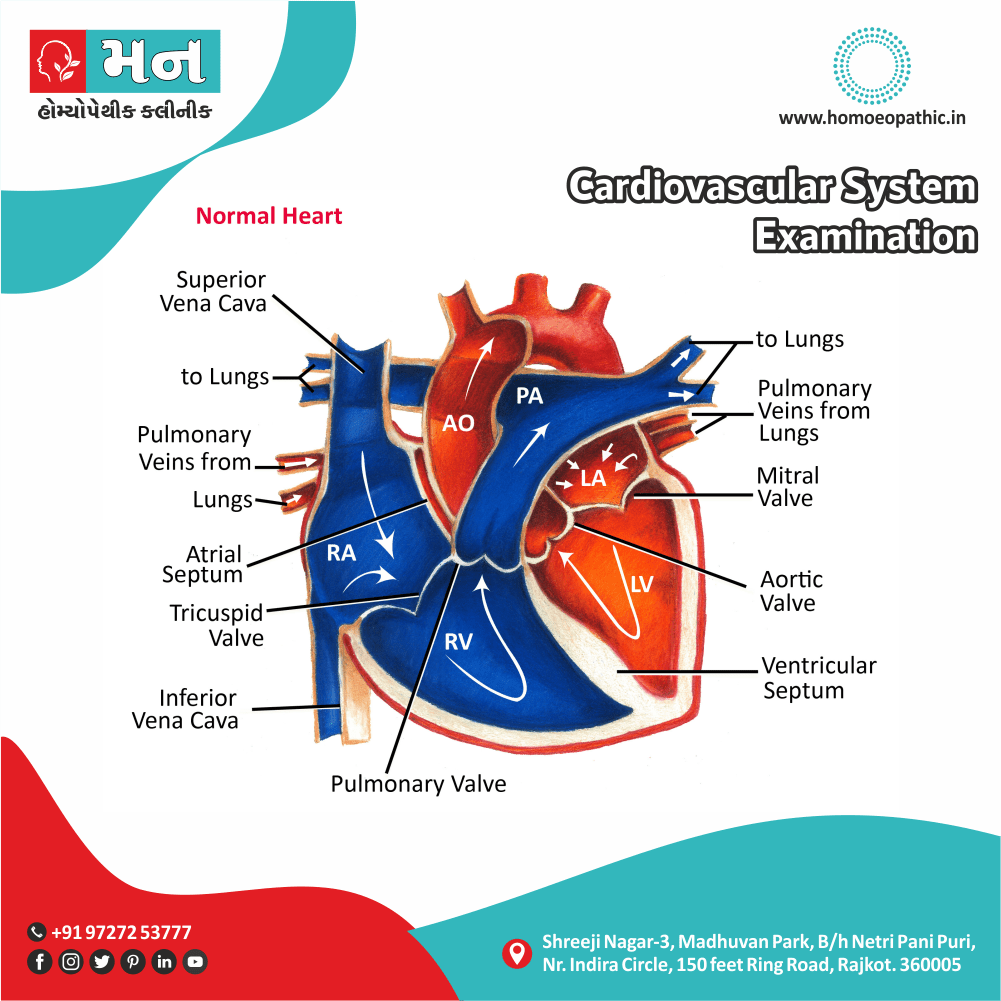
- Cardio-vascular examination: Examination of cardiovascular system is crucial in management of delirium.
- Careful heart auscultation may reveal underlying pathology.
- Frictional rub may suggest pericarditis.
- New onset murmur may be indicative of myocardial infarction.
- Pulmonary examination: Depressed respiration may be suggestive of drug overdose.
- Basal rales may be suggestive of cardiac failure.
- wheeze may be because of asthma or COPD.
- Increased tactile, vocal fermitus, egophony and dull on percussion may indicate underlying pneumonia.
- Abdominal examination:
- Ascitis may be suggestive of hepatic, renal or cardiac pathology.
- Organomegaly may be indicative of portal hypertension and hepatic pathology.(6)
Diagnosis of Delirium
The diagnosis is clinical and is usually obvious upon talking to the patient. Typically, a standard medical and surgical history is take, rather than a formal psychiatric interview. Often little history can be obtained from the patient, so it is essential to contact relatives, carers, friends, and other clinicians in order to gather the story.
Include a comprehensive list of medications, including over-the-counter remedies, alcohol, also smoking. All in all, a full examination of all physical systems should undertake, including a detailed neurological examination.
Physical investigations should include the following:
- Blood for full blood count, urea and electrolytes, liver function tests, thyroid function tests, calcium, phosphate, magnesium, glucose, lactate, troponin, albumin, paracetamol also salicylate, haematinics;
- Blood also urine cultures;
- Arterial blood gas;
- ECG;
- Urinalysis;
- Chest X-ray;
- Consider further tests, e.g. CT head, lumbar puncture, EEG.
- Abbreviated Mental Test Score (AMTS): Out of 10 points, a score of 6 or less is taken as delirium.
- Mini Mental State Examination (MMSE): 30 points, with more than or equal to 25 taken as normal, mild dementia 21–24, moderate 10–20, and severe less than 10 points. [1]
Differential diagnosis of Delirium
- Psychiatric Disorders
- Dementia
- Alzheimer disease
- Depression
- Dementia
- Pain
- Stroke and transient ischaemic attack
- Myocardial infarction
- Traumatic head injury
- Adrenal crisis
- Thyrotoxicosis
- Myxoedema coma (6)
Treatment of Delirium
1. Treat the underlying cause:
This obviously depends on the exact aetiology, but frequently involves giving oxygen, fluids, antibiotics, and pain relief, as well as any specific treatments. Intravenous access (and other invasive procedures) should only be undertaken if there is a valid indication.
2. Reassurance and reorientation:
Patients need reassurance to reduce anxiety and disorientation; this should be repeated frequently. A clock should be visible at all times, and the patient reminded of the time, place, day, and date regularly.
3. Predictable, consistent routine:
On the ward the patient should be nursed either in a quiet side room or next to the nursing station. It should be reasonably dark at night and light during the day. Meals and activities should occur at standard times each day. Relatives and friends should be encouraged to stay or to visit frequently.
4. Avoid unnecessary medications.
5. Explain to relatives and friends:
what delirium is and what has caused it. This helps them to reassure and reorientate the patient.
6. Sleep:
It is often disturb, and it is reasonable to give small doses of hypnotics (e.g. zopiclone 3.75 mg) or benzodiazepines (e.g. temazepam 10 mg) at night to promote sleep. Benzodiazepines should avoide during daytime as their sedative effects may increase disorientation. The exception to this is in alcohol withdrawal or in order to treat seizures.
7. Disturbed, violent, or distressed behaviour:
It may treat with carefully monitored antipsychotic medications. Additionally, There is good randomized control evidence supporting the use of antipsychotics in delirium, with a consistent two thirds of patients experiencing clinical improvement.
Haloperidol is the traditional choice, 0.25–2 mg every 4 hours, although atypical antipsychotics are becoming more commonly use. Haloperidol is available in oral, intramuscular, and intravenous preparations.
Olanzapine has shown to be just as effective at relieving agitation as haloperidol, but the intramuscular formulation is not widely available.
Lorazepam is also effective, but has a moderate risk of worsening the mental state. If a patient is acutely distress or agitate, an IM dose is usually needed, with follow-on treatment orally for as long as necessary.
This should be regularly reviewed, and never used unless other methods of management have been exhausted. [1]
Prevention of Delirium
- Communicate clearly and address sensory impairment
- Minimise the patient’s confusion
- Encourage mobility and self-care
- Optimise nutrition, hydration and regular continence
- Minimise risk of injury and agitation
- Minimise use of antipsychotic medications
- Monitor and respond to pain
- Use night-time strategies to promote sleep
Homeopathic Treatment of Delirium
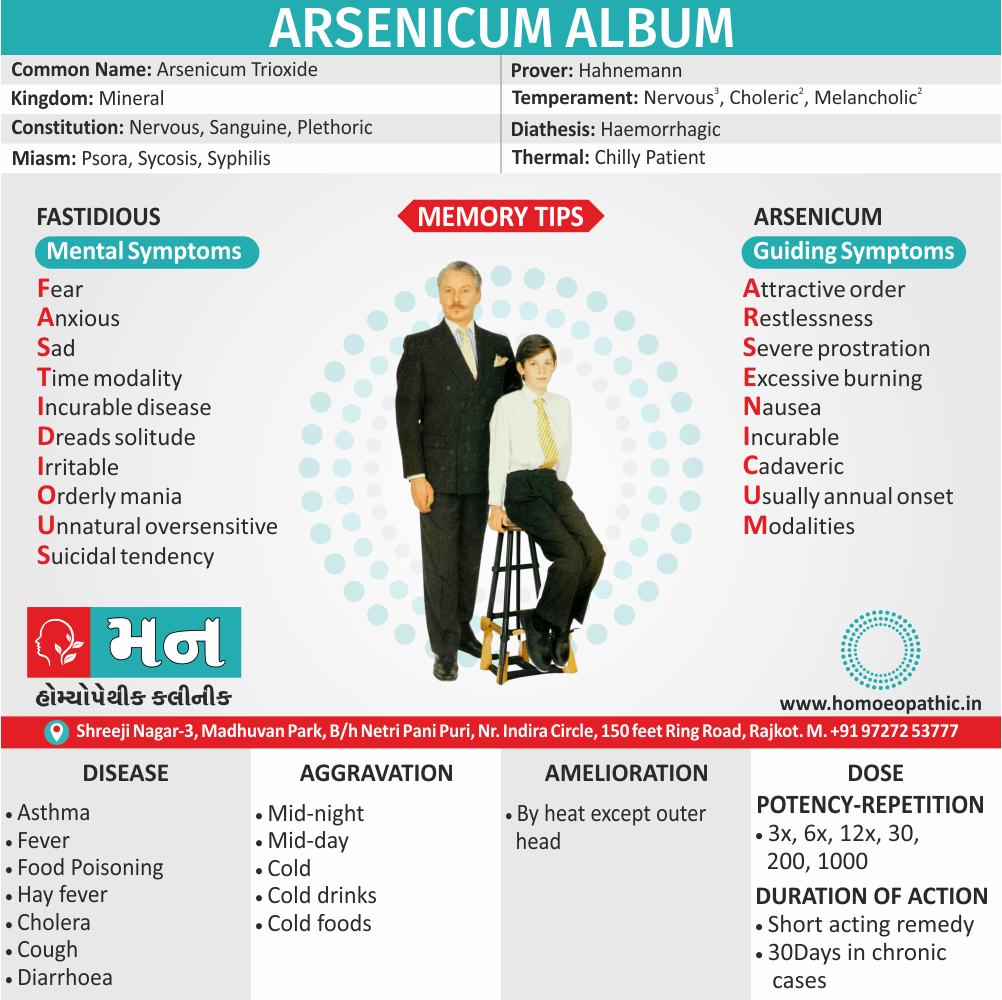
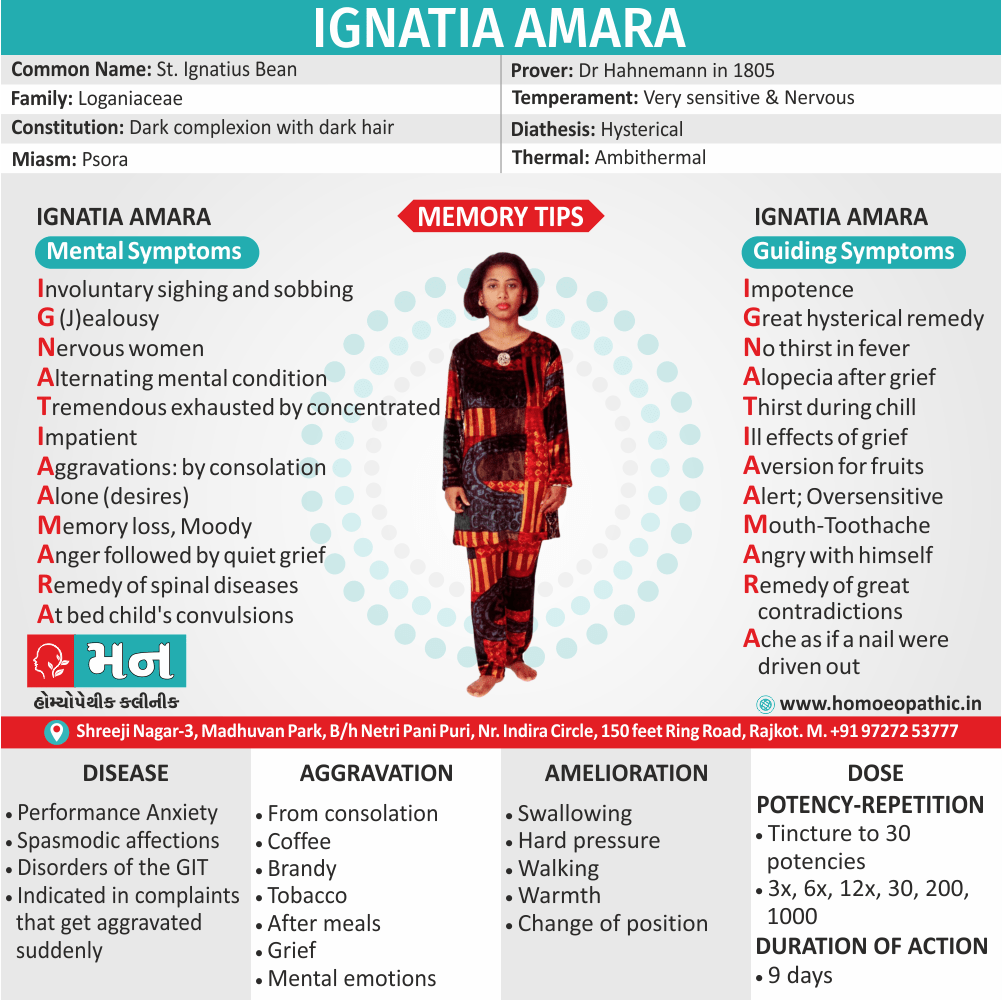
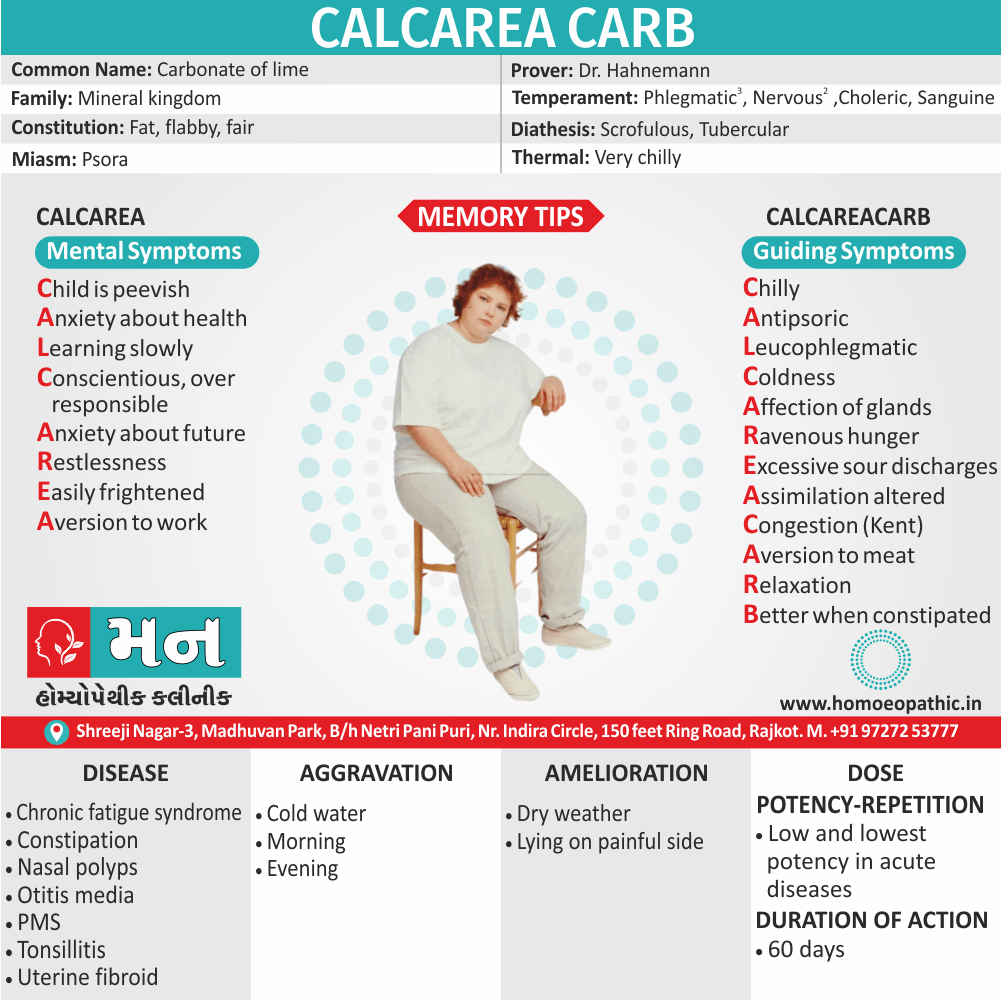
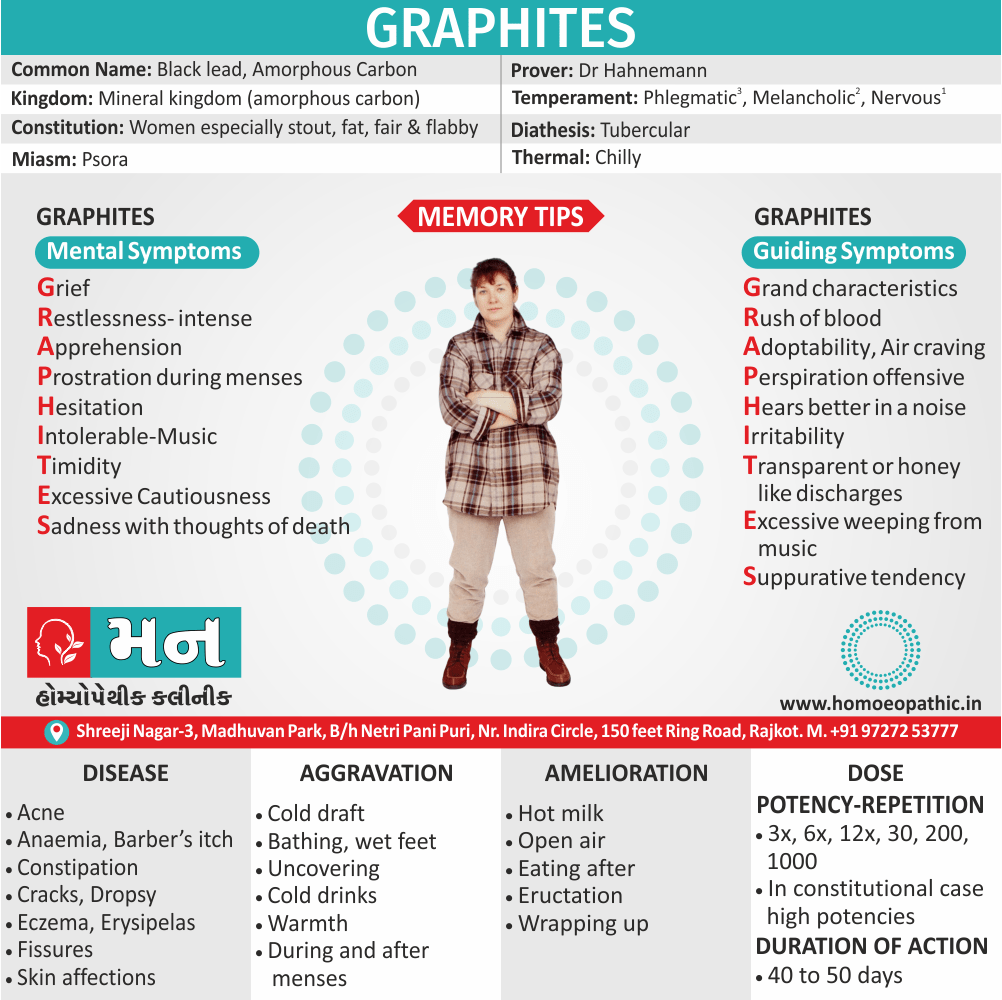
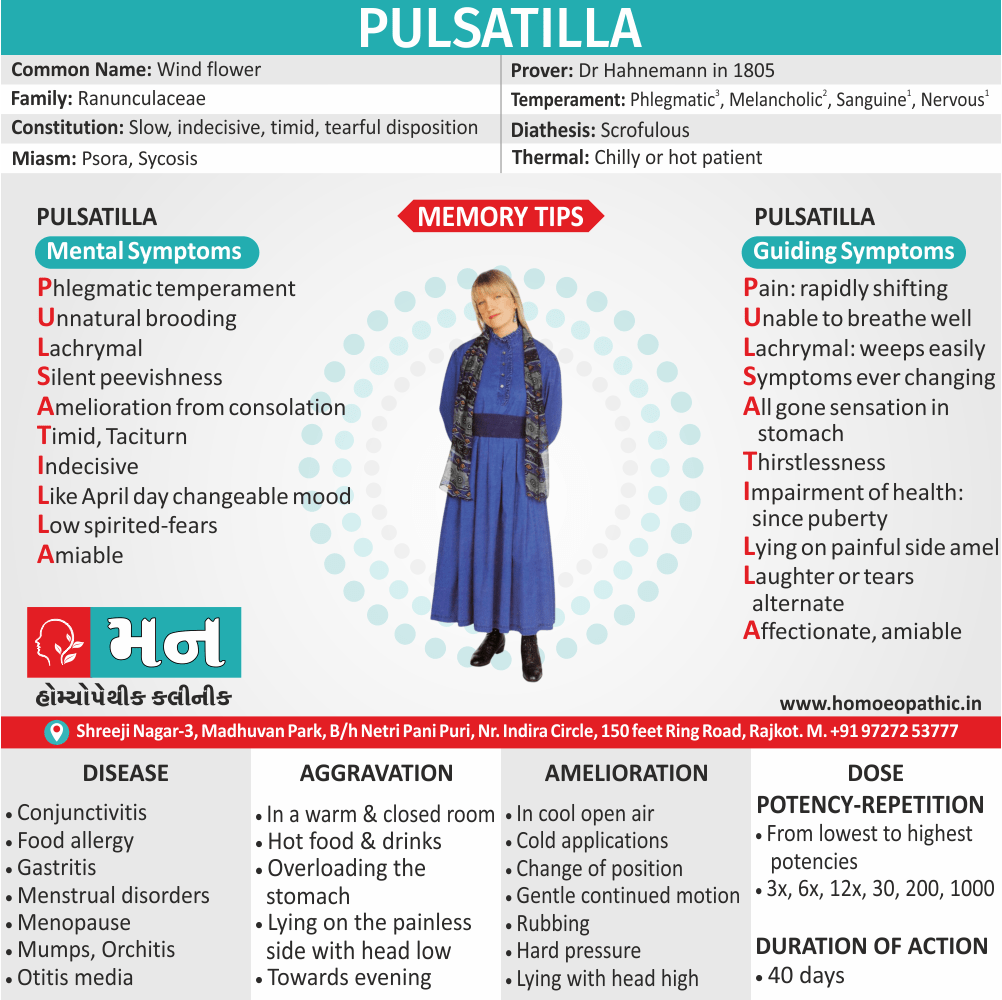
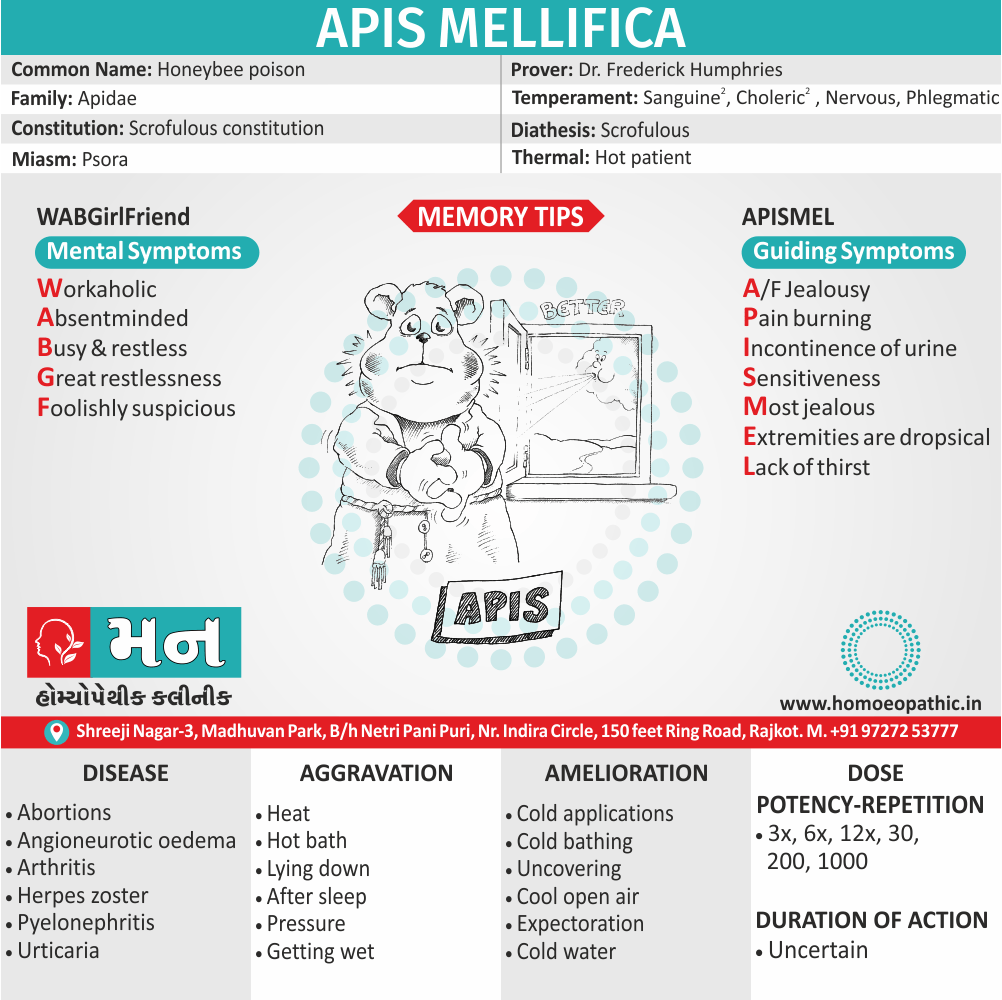
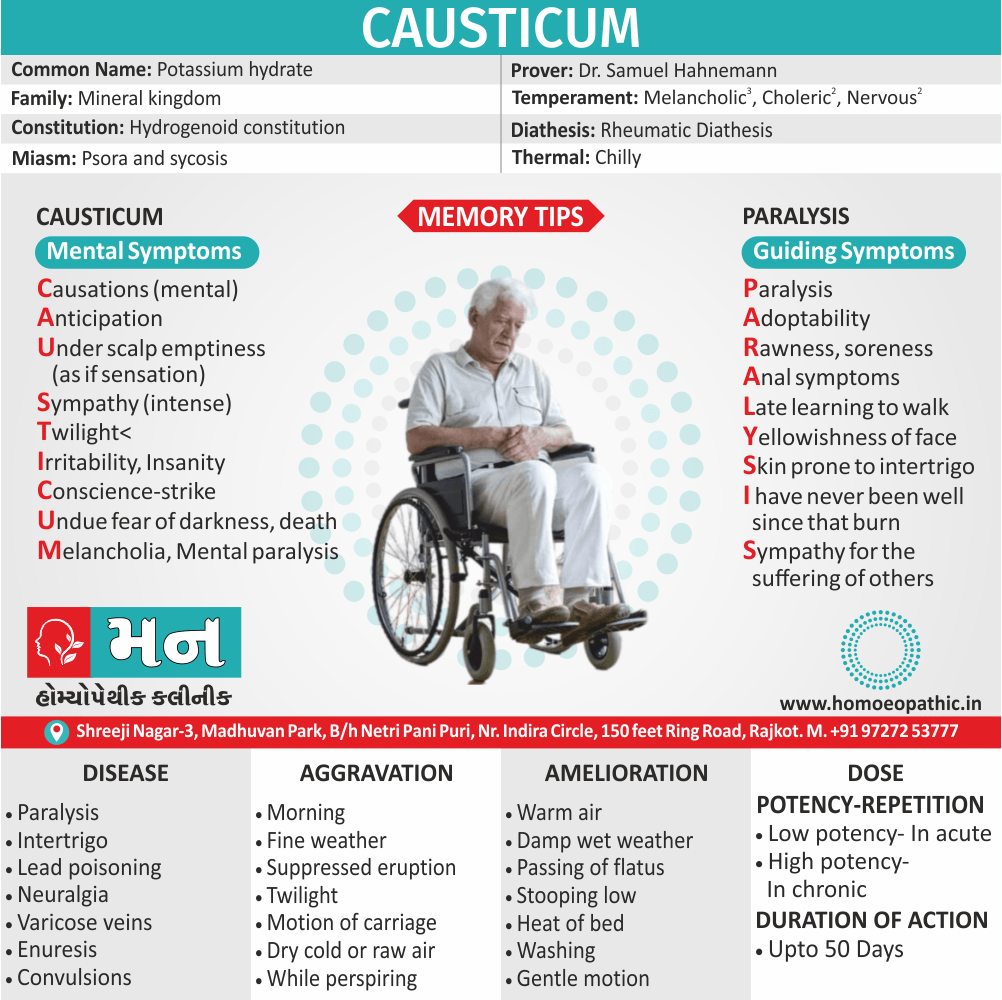
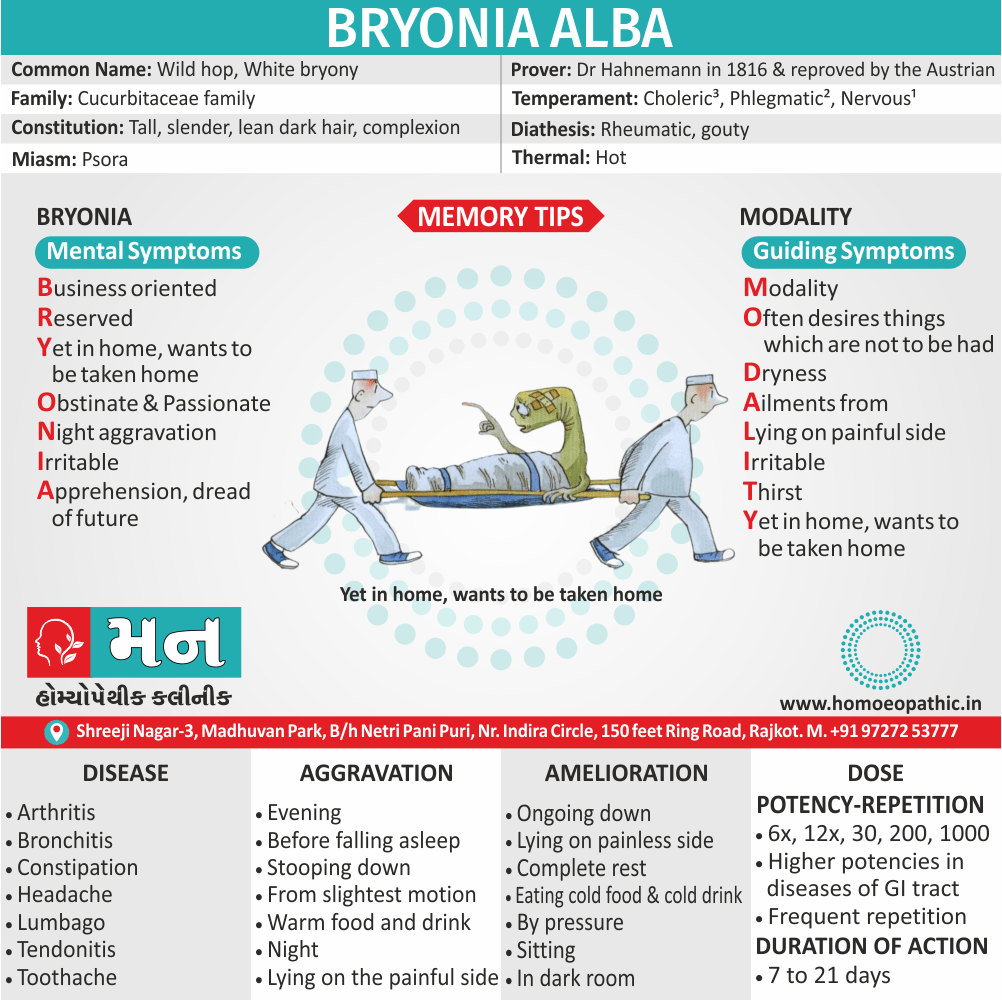
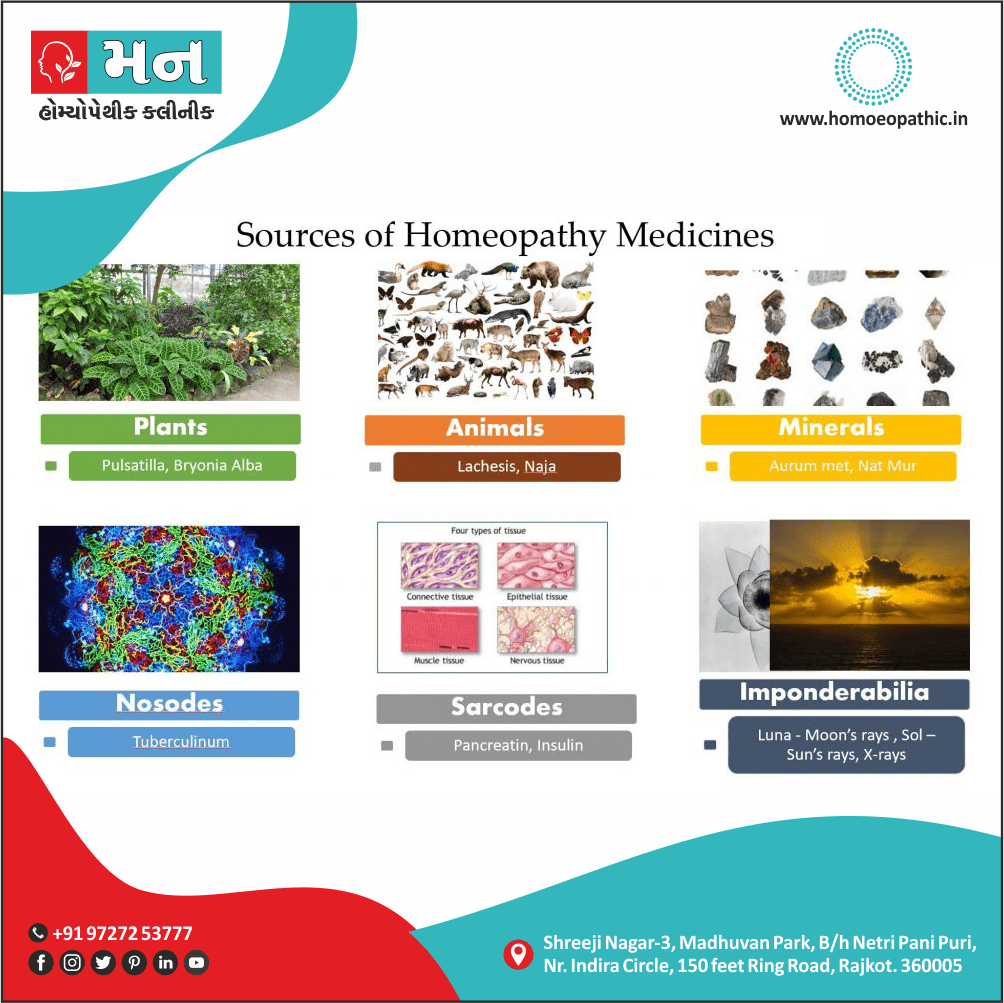
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
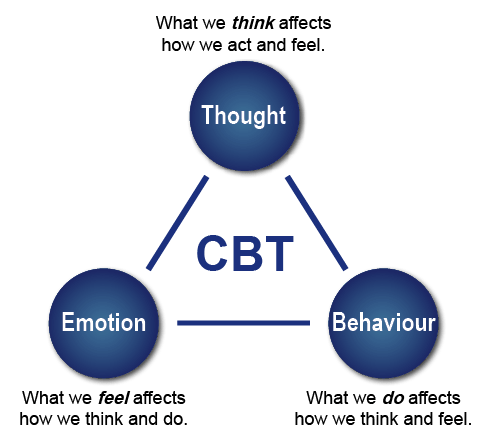
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Delirium:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
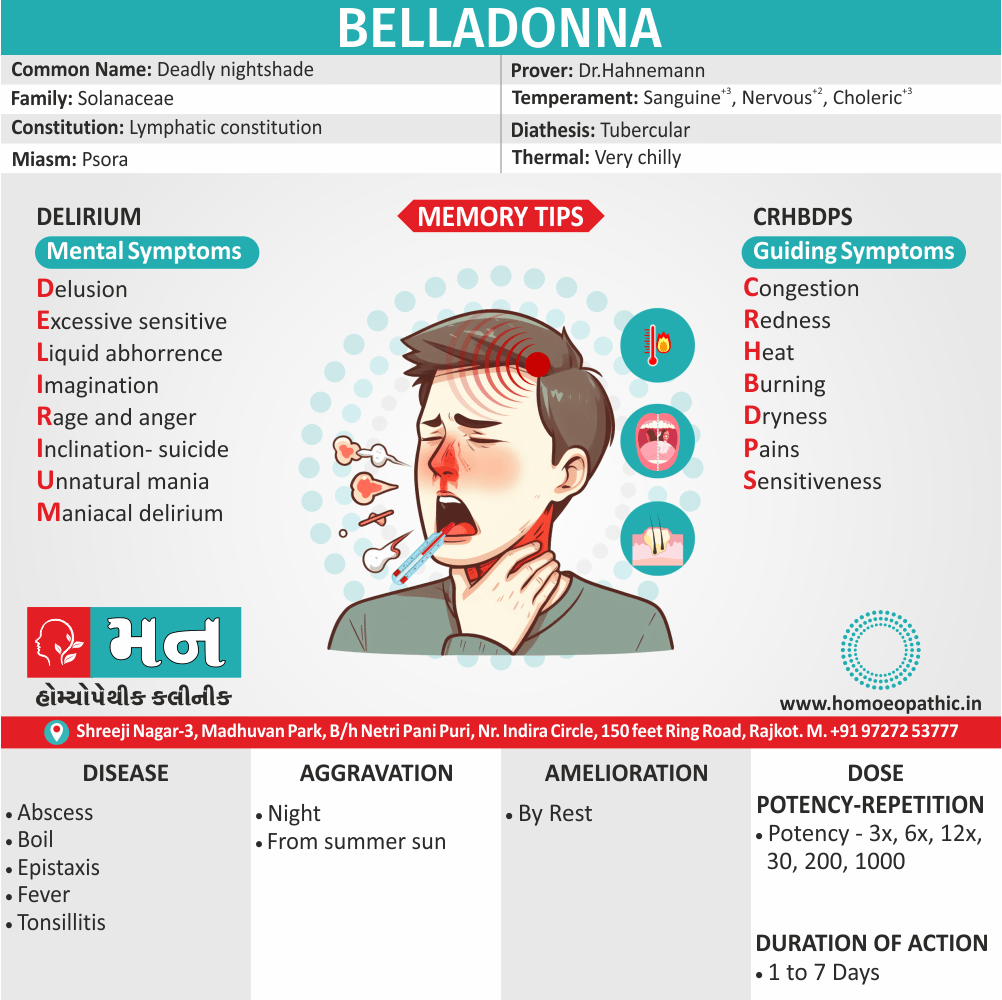
Belladonna:
Generally, Belladonna comes to mind first in delirium. Moreover, It has a violent delirium with loud laughing screaming out, and grinding of the teeth, and, as in all narcotics, a desire to hide or escape. Additionally, The patient is full of fears and imaginings, also the delirium manifests itself by the most positive ebullitions of rage and fury. Besides this, Its general character is one of great activity with great excitement, a hot face and head and oftentimes there is present a sensation as if falling and the patient clutches the air. Sometimes there is a stupor, and when aroused they strike people bark and bite like a dog and are most violent.
Hyoscyamus:
This remedy has not the intensely high degree of maniacal excitement that we find under Stramonium, nor has it the cerebral congestion that characterizes Belladonna. With Hyoscyamus there is an aversion especially, to light, and the patient fears being poisoned; he will sit up in bed, talk and mutter all the time, and look wildly about him. There is a great deal of nervousness, whining, crying also twitching; he tries to escape from imaginary foes; a constant picking at the bedclothes and objects in the air is most characteristic. All in all, It is the remedy for that curious condition of delirium known as "coma vigil."
Stramonium:
Specifically, with this remedy the delirium is more furious, the mania more acute and the sensorium more perverted and excited than under Belladonna or Hyoscyamus. Furthermore, the patient desires light and company, is very loquacious, garrulous, laughs, sings, swears, prays, curses also makes rhymes. Besides this, He sees ghosts, talks . with spirits and hears voices. Lastly, the head is raised frequently from the pillow, the face is bright· red, also he has a terrified expression; in fact, he seems to see objects rising from every corner to frighten him. Sometimes a silly delirium is present.
Lachesis:
Is characterized by great talkativeness in delirium. It has also the fear of being poisoned; but the Lachesis delirium is of a low form accompanied by dropping of the lower jaw, also a characteristic is that they imagine them- selves under some super-human control.
Cimicifuga:
This remedy has loquacity, with a continual changing of the subject when talking, imaginings of rats, mice, etc. It is usually dependent upon uterine disease.
Veratrum album:
Veratrum has restlessness, and a desire to cut and tear the clothing as in Belladonna; but with this remedy there is a coldness of the surface of the body and a cold sweat. The patient is loquacious, talks very loud and is frightened at imaginary things. It also has a state of frenzy or excitement, during which he indulges in shrieks, in expressions of fright and in violent cursings of those around him.
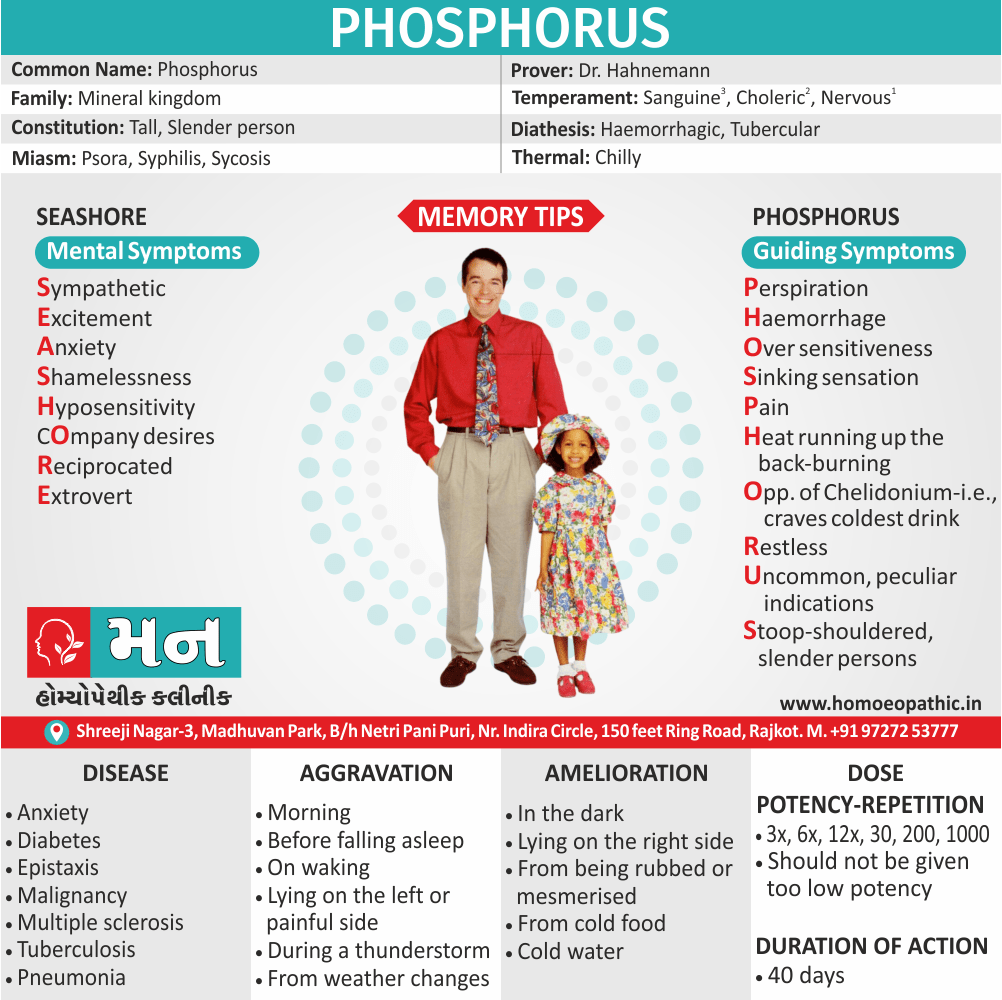
Phosphorus:
The delirium of Phosphorus is of a low typhoid type, with tendency to haemorrhage and an apathetic, sluggish, stupid state, where the patient is unwilling to talk and answers question slowly. It has also an ecstatic state, in which he sees all sorts of faces grinning at him. He has also imaginary notions, such as imagining that his body is in fragments.
Baptisia:
Generally, The patient imagines his body either in pieces or double: and scattered about, also he has to move constantly to keep the pieces together.
Thuja:
In brief, Here the patient imagines that he is made of glass and moves carefully for fear of breaking.
Absinthium:
Basically, patient has a delirium with a constant desire to move about.
Agaricus:
Dr Bayes praises this remedy highly in the delirium especially, of typhoid fever, where there are constant attempts to get out of bed and tremor of the whole body. [3]
Frequently Asked Questions
What is Delirium?
Delirium is an acute generalize impairment of brain function, in which the most important feature is impairment of consciousness.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Delirium?
- Belladonna
- Hyoscyamus
- Stramonium
- Lachesis
- Cimicifuga
- Veratrum album
- Phosphorus
- Baptisia
- Thuja
- Agaricus
What are the main signs of Delirium?
- Impaired consciousness
- Disorientation
- Poor attention and concentration
- Loss of memory Behaviour
- Overactive
- Under active Thinking
- Muddled (in other words, confused)
- Ideas of reference
- Delusions Mood
- Anxious, irritable
- Depressed
- Perplexed
- Perception
- Misinterpretations
- Hallucinations, mainly visual
What are the causes of Delirium?
- Hypoxia
- Hypoglycaemia
- Hepatic encephalopathy
- Cardiac failure
- Hypo- and Hyperthyroidism
- Digitalis, Quinidine, Antihypertensives
- Alcohol, Sedatives, Hypnotics
- Anticonvulsants
- Proteins Systemic Infections
- Epilepsy
- Head injury
Reference
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 26.
- A Short Textbook of Psychiatry by Niraj Ahuja /Ch 3.
- Homeopathy in Treatment Of Psychological Disorders by Shilpa Harwani / Ch 17.
- Delirium risk factors | CHOPs (nsw.gov.au)
- Delirium – Symptoms and causes – Mayo Clinic
Delirium:
Definition:
Delirium is the commonest organic mental disorder in clinical practice. [2]
Delirium is an acute generalize impairment of brain function, in which the most important feature is impairment of consciousness. The disturbance of brain function is generalized, and the primary cause is often outside the brain; for example, sepsis due to a urinary tract infection. [1]
Frequently Asked Questions (FAQ)
XYZ
XXX
XYZ
XXX
XYZ
XXX
People found Homeopathic Clinic For XXXX by searching for
XXX
People found Homeopathic Doctors for XXXX by searching for
XXX
People found Homeopathic treatment for XXXX by searching for
XXX
Overview
Epidemiology
Causes
Risk Factors
Types
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Dont’s
Terminology
References
FAQ
Also Search As
Overview
Epidemiology
Indian epidemiology then other
Causes
Causes of Delirium
Metabolic Causes:
i. Hypoxia, Carbon dioxide narcosis
ii. Hypoglycaemia
iii. Hepatic encephalopathy, Uremic encephalopathy
iv. Cardiac failure, Cardiac arrhythmias, Cardiac arrest
v. Water and electrolyte imbalance (e.g. Water, Na+, K+, Mg++, Ca++)
vi. Metabolic acidosis or alkalosis
vii. Fever, Anaemia, Hypovolemic shock
viii. Carcinoid syndrome, Porphyria
viii. Carcinoid syndrome, Porphyria
Endocrine Causes:
i. Hypo- and Hyperpituitarism
ii. Hypo- and Hyperthyroidism
iii. Hypo- and Hyperparathyroidism
iv. Hypo- and Hyperadrenalism
Drugs (Both ingestion and withdrawal can cause delirium) and Poisons:
i. Digitalis, Quinidine, Antihypertensives
ii. Alcohol, Sedatives, Hypnotics (especially barbiturates)
iii. Tricyclic antidepressants, Antipsychotics, Anticholinergics, Disulfiram
iv. Anticonvulsants,, L-dopa, Opiates
v. Salicylates, Steroids, Penicillin, Insulin
vi. Methyl alcohol, heavy metals, biocides
Nutritional Deficiencies:
i. Thiamine, Niacin, Pyridoxine, Folic acid, B12
ii. Proteins Systemic Infections i. Acute and Chronic, e.g. Septicaemia, Pneumonia, Endocarditis
Intracranial Causes:
i. Epilepsy (i.e. postictal states)
ii. Head injury, Subarachnoid haemorrhage, Subdural haematoma
iii. Intracranial infections, e.g. Meningitis, Encephalitis, Cerebral malaria
iv. Migraine
v. Stroke (especially; acute phase), Hypertensive encephalopathy
vi. Focal lesions, e.g. right parietal lesions (such as abscess, neoplasm)
Miscellaneous:
i. Postoperative states (including ICU delirium) ii. Sleep deprivation iii. Heat, Electricity, Radiation. [2]
Risk Factors
Risk factors are things that make you more likely to develop a disease in the first place.
Risk factors of Delirium
- Pre-existing dementia
- Severe medical Illness
- History of previous delirium
- Visual and hearing impairment
- Depression
- Abnormal sodium, potassium and glucose
- Polypharmacy
- Alcohol/ Benzodiazepine use
- Use of physical restraint
- Use of indwelling catheter
- Adding three or more medications
- Multiple bed moves
- Pain
- Surgery
- Anaesthesia and hypoxia
- Malnutrition and dehydration (4)
Types
Types of delirium
Experts have identified three types:
- Hyperactive delirium- This may be the easiest type to recognize. People with this type may be restless and pace the room. They also may be anxious, have rapid mood swings or see things that aren’t there. People with this type often resist care.
- Hypoactive delirium- People with this type may be inactive or have reduced activity. They tend to be sluggish or drowsy. They might seem to be in a daze. They don’t interact with family or others.
- Mixed delirium- Symptoms involve both types of delirium. The person may quickly switch back and forth from being restless and sluggish. (5)
Pathophysiology
Pathophysiology of Delirium
The pathophysiology of delirium remains relatively unclear. In general, neuroimaging studies reveal disruptions in higher cortical functioning in multiple disparate areas of the brain, including the prefrontal cortex, subcortical structures, thalamus, basal ganglia, lingual gyri, and frontal, fusiform, and temporoparietal cortex.
Electroencephalographic (EEG) studies also show diffuse slowing of cortical activity.
Theories on the pathogenesis of delirium point to the role of neurotransmitters, inflammation, and chronic stress on the brain. For example, the role of cholinergic deficiency in inducing delirium is strengthened by the clear association of anticholinergic drug use with increased incidence. Studies in surgical patients have demonstrated a dysfunctional interaction between the cholinergic and immune systems in patients who developed postoperative delirium.
Dopaminergic excess is also believed to contribute. Evidence does not appear to support the use of antipsychotic medications (dopamine antagonists) for the prevention or treatment of delirium but is not entirely consistent.
Other neurotransmitters implicated in the pathophysiology of delirium include noradrenaline, serotonin, gamma-aminobutyric acid, glutamate, and melatonin.
Evidence also points to the role of cytokines such as interleukins 1 and 2 and TNF-alpha and interferon in contributing to delirium.
Finally, chronic hypercortisolism, as induced by chronic stress secondary to illness or trauma, may also contribute to delirium initiation.(6)
Clinical Features
Tab Content
Sign & Symptoms
Sign & Symptoms of Delirium
- Impaired consciousness
- Disorientation
- Poor attention also concentration
- Loss of memory Behaviour
- Overactive
- Under active Thinking
- Muddled (in other words, confused)
- Ideas of reference
- Delusions Mood
- Anxious, irritable
- Depressed
- Perplexed
- Perception
- Misinterpretations
- Hallucinations, mainly visual
- Acute onset, fluctuating course, worse especially, in the evening
Impairment of consciousness is the most important symptom, and is seen as a deficit of attention, concentration, and awareness. Furthermore, Often the patient will not be able to follow or engage in a logical conversation. All in all, The features fluctuate in intensity and are often worse in the evening.
Disorientation: Uncertainty about the time, place, also identity of other people.
Behaviour may be either overactive, with noisiness and irritability, or underactive. Besides this, Sleep is often disturbed.
Thinking is slow and confused but the content is often complex. Ideas of reference also delusions are common.
Mood may anxious, perplex, either irritable or depress and is often labile.
Perception may distort with misinterpretations, illusions, and visual hallucinations. Additionally, Tactile and auditory hallucinations occur but are less frequent.
Memory : Generally, Disturbance of memory affects registration, retention, and recall, as well as new learning.
Insight is impaired. [1]
Clinical Examination
Clinical examination of Delirium
- Delirium symptom changes in severity during its course.
- It is essential to assess the patient multiple times, as it is easy to miss a diagnosis, also features like sundowning can be overlooked if the assessment is not done towards the end of the day.
General Examination
- Vital signs:
- Pulse: Increased pulse rate may be suggestive of heat failure, myocardial infarction or pulmonary pathology.
- Blood pressure: Malignant hypertension is an important cause of delirium, and blood pressure must be monitored if the patient is non compliant with antihypertensive medications.
- Low blood pressure may suggest heart failure.
- Appearance:
- Cherry red color indicates carbon monoxide poisoning,
- cyanosis may indicate respiratory or cardiac pathology.
- Jaundice may indicate hepatic or biliary pathology.
- Edema may be because of liver failure, cardiac failure, renal failure or malnutrition.
- Temperature:
- Fever may indicate underlying infection.
- Conscious level:
- Various levels of arousal can be seen in delirium, ranging from stupor to hyperarousal. If the patient appears to have a normal arousal level, attention deficit must be accessed which is very commonly seen in delirium.
- Cognitive function using a standardized screening tool, e.g. MoCA, Mini mental state examination or 4AT.
- Nutritional status: B12 and folate deficiencies can be assessed on physical examination.
- Hydration state: Dehydration as well as an overload of fluids, resulting in hypoxia can cause delirium.
- Infectious foci: Careful examination to rule out conditions such as meningitis, encephalitis, pulmonary consolidation etc.
- Evidence of intoxication or withdrawal for alcohol, and recreational drugs are an important part of delirium work up. Look for tremors, pupil size, needle tracks etc.
Systemic Examination
- Focused examination is necessary to find out underlying etiology.
- Neurological examinations: Careful examination must be done to find out neurological causes of delirium, such as cerebrovascular diseases, neurodegenrative disorders such as parkinsonism, Alzheimer, and lewi body dementia.
- Many systemic diseases may show neurological manifestations: hepatic encephalopathy causes flapping tremor.
- Overdose and intoxication can also effect the central nervous system : opiates causes pinpoint pupils and respiratory depression.
- Cardio-vascular examination: Examination of cardiovascular system is crucial in management of delirium.
- Careful heart auscultation may reveal underlying pathology.
- Frictional rub may suggest pericarditis.
- New onset murmur may be indicative of myocardial infarction.
- Pulmonary examination: Depressed respiration may be suggestive of drug overdose.
- Basal rales may be suggestive of cardiac failure.
- wheeze may be because of asthma or COPD.
- Increased tactile, vocal fermitus, egophony and dull on percussion may indicate underlying pneumonia.
- Abdominal examination:
- Ascitis may be suggestive of hepatic, renal or cardiac pathology.
- Organomegaly may be indicative of portal hypertension and hepatic pathology.(6)
Diagnosis
Diagnosis of Delirium
The diagnosis is clinical and is usually obvious upon talking to the patient. Typically, a standard medical and surgical history is take, rather than a formal psychiatric interview. Often little history can be obtained from the patient, so it is essential to contact relatives, carers, friends, and other clinicians in order to gather the story.
Include a comprehensive list of medications, including over-the-counter remedies, alcohol, also smoking. All in all, a full examination of all physical systems should undertake, including a detailed neurological examination.
Differential Diagnosis
Differential diagnosis of Delirium
- Psychiatric Disorders
- Dementia
- Alzheimer disease
- Depression
- Dementia
- Pain
- Stroke and transient ischaemic attack
- Myocardial infarction
- Traumatic head injury
- Adrenal crisis
- Thyrotoxicosis
- Myxoedema coma (6)
Complications
Complications are what happen after you have a disease. They are the negative consequences of the disease process.
Investigations
Diagnosis of Delirium
The diagnosis is clinical and is usually obvious upon talking to the patient. Typically, a standard medical and surgical history is take, rather than a formal psychiatric interview. Often little history can be obtained from the patient, so it is essential to contact relatives, carers, friends, and other clinicians in order to gather the story.
Include a comprehensive list of medications, including over-the-counter remedies, alcohol, also smoking. All in all, a full examination of all physical systems should undertake, including a detailed neurological examination.
Physical investigations should include the following:
- Blood for full blood count, urea and electrolytes, liver function tests, thyroid function tests, calcium, phosphate, magnesium, glucose, lactate, troponin, albumin, paracetamol also salicylate, haematinics;
- Blood also urine cultures;
- Arterial blood gas;
- ECG;
- Urinalysis;
- Chest X-ray;
- Consider further tests, e.g. CT head, lumbar puncture, EEG.
- Abbreviated Mental Test Score (AMTS): Out of 10 points, a score of 6 or less is taken as delirium.
- Mini Mental State Examination (MMSE): 30 points, with more than or equal to 25 taken as normal, mild dementia 21–24, moderate 10–20, and severe less than 10 points. [1]
Treatment
Treatment of Delirium
1. Treat the underlying cause:
This obviously depends on the exact aetiology, but frequently involves giving oxygen, fluids, antibiotics, and pain relief, as well as any specific treatments. Intravenous access (and other invasive procedures) should only be undertaken if there is a valid indication.
2. Reassurance and reorientation:
Patients need reassurance to reduce anxiety and disorientation; this should be repeated frequently. A clock should be visible at all times, and the patient reminded of the time, place, day, and date regularly.
3. Predictable, consistent routine:
On the ward the patient should be nursed either in a quiet side room or next to the nursing station. It should be reasonably dark at night and light during the day. Meals and activities should occur at standard times each day. Relatives and friends should be encouraged to stay or to visit frequently.
4. Avoid unnecessary medications.
5. Explain to relatives and friends:
what delirium is and what has caused it. This helps them to reassure and reorientate the patient.
6. Sleep:
It is often disturb, and it is reasonable to give small doses of hypnotics (e.g. zopiclone 3.75 mg) or benzodiazepines (e.g. temazepam 10 mg) at night to promote sleep. Benzodiazepines should avoide during daytime as their sedative effects may increase disorientation. The exception to this is in alcohol withdrawal or in order to treat seizures.
7. Disturbed, violent, or distressed behaviour:
It may treat with carefully monitored antipsychotic medications. Additionally, There is good randomized control evidence supporting the use of antipsychotics in delirium, with a consistent two thirds of patients experiencing clinical improvement.
Haloperidol is the traditional choice, 0.25–2 mg every 4 hours, although atypical antipsychotics are becoming more commonly use. Haloperidol is available in oral, intramuscular, and intravenous preparations.
Olanzapine has shown to be just as effective at relieving agitation as haloperidol, but the intramuscular formulation is not widely available.
Lorazepam is also effective, but has a moderate risk of worsening the mental state. If a patient is acutely distress or agitate, an IM dose is usually needed, with follow-on treatment orally for as long as necessary.
This should be regularly reviewed, and never used unless other methods of management have been exhausted. [1]
Prevention
Prevention of Delirium
- Communicate clearly and address sensory impairment
- Minimise the patient’s confusion
- Encourage mobility and self-care
- Optimise nutrition, hydration and regular continence
- Minimise risk of injury and agitation
- Minimise use of antipsychotic medications
- Monitor and respond to pain
- Use night-time strategies to promote sleep
Homeopathic Treatment
Homeopathic Treatment of Delirium
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Delirium:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Belladonna:
Generally, Belladonna comes to mind first in delirium. Moreover, It has a violent delirium with loud laughing screaming out, and grinding of the teeth, and, as in all narcotics, a desire to hide or escape. Additionally, The patient is full of fears and imaginings, also the delirium manifests itself by the most positive ebullitions of rage and fury. Besides this, Its general character is one of great activity with great excitement, a hot face and head and oftentimes there is present a sensation as if falling and the patient clutches the air. Sometimes there is a stupor, and when aroused they strike people bark and bite like a dog and are most violent.
Hyoscyamus:
This remedy has not the intensely high degree of maniacal excitement that we find under Stramonium, nor has it the cerebral congestion that characterizes Belladonna. With Hyoscyamus there is an aversion especially, to light, and the patient fears being poisoned; he will sit up in bed, talk and mutter all the time, and look wildly about him. There is a great deal of nervousness, whining, crying also twitching; he tries to escape from imaginary foes; a constant picking at the bedclothes and objects in the air is most characteristic. All in all, It is the remedy for that curious condition of delirium known as "coma vigil."
Stramonium:
Specifically, with this remedy the delirium is more furious, the mania more acute and the sensorium more perverted and excited than under Belladonna or Hyoscyamus. Furthermore, the patient desires light and company, is very loquacious, garrulous, laughs, sings, swears, prays, curses also makes rhymes. Besides this, He sees ghosts, talks . with spirits and hears voices. Lastly, the head is raised frequently from the pillow, the face is bright· red, also he has a terrified expression; in fact, he seems to see objects rising from every corner to frighten him. Sometimes a silly delirium is present.
Lachesis:
Is characterized by great talkativeness in delirium. It has also the fear of being poisoned; but the Lachesis delirium is of a low form accompanied by dropping of the lower jaw, also a characteristic is that they imagine them- selves under some super-human control.
Cimicifuga:
This remedy has loquacity, with a continual changing of the subject when talking, imaginings of rats, mice, etc. It is usually dependent upon uterine disease.
Veratrum album:
Veratrum has restlessness, and a desire to cut and tear the clothing as in Belladonna; but with this remedy there is a coldness of the surface of the body and a cold sweat. The patient is loquacious, talks very loud and is frightened at imaginary things. It also has a state of frenzy or excitement, during which he indulges in shrieks, in expressions of fright and in violent cursings of those around him.
Phosphorus:
The delirium of Phosphorus is of a low typhoid type, with tendency to haemorrhage and an apathetic, sluggish, stupid state, where the patient is unwilling to talk and answers question slowly. It has also an ecstatic state, in which he sees all sorts of faces grinning at him. He has also imaginary notions, such as imagining that his body is in fragments.
Baptisia:
Generally, The patient imagines his body either in pieces or double: and scattered about, also he has to move constantly to keep the pieces together.
Thuja:
In brief, Here the patient imagines that he is made of glass and moves carefully for fear of breaking.
Absinthium:
Basically, patient has a delirium with a constant desire to move about.
Agaricus:
Dr Bayes praises this remedy highly in the delirium especially, of typhoid fever, where there are constant attempts to get out of bed and tremor of the whole body. [3]
Diet & Regimen
Do’s and Dont’s
Tab Content
Terminology
Tab Content
References
Reference
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 26.
- A Short Textbook of Psychiatry by Niraj Ahuja /Ch 3.
- Homeopathy in Treatment Of Psychological Disorders by Shilpa Harwani / Ch 17.
- Delirium risk factors | CHOPs (nsw.gov.au)
- Delirium – Symptoms and causes – Mayo Clinic
FAQ
Frequently Asked Questions
What is Delirium?
Delirium is an acute generalize impairment of brain function, in which the most important feature is impairment of consciousness.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Delirium?
- Belladonna
- Hyoscyamus
- Stramonium
- Lachesis
- Cimicifuga
- Veratrum album
- Phosphorus
- Baptisia
- Thuja
- Agaricus
What are the main signs of Delirium?
- Impaired consciousness
- Disorientation
- Poor attention and concentration
- Loss of memory Behaviour
- Overactive
- Under active Thinking
- Muddled (in other words, confused)
- Ideas of reference
- Delusions Mood
- Anxious, irritable
- Depressed
- Perplexed
- Perception
- Misinterpretations
- Hallucinations, mainly visual
What are the causes of Delirium?
- Hypoxia
- Hypoglycaemia
- Hepatic encephalopathy
- Cardiac failure
- Hypo- and Hyperthyroidism
- Digitalis, Quinidine, Antihypertensives
- Alcohol, Sedatives, Hypnotics
- Anticonvulsants
- Proteins Systemic Infections
- Epilepsy
- Head injury