Osteoarthritis-OA
Definition of Osteoarthritis-OA:
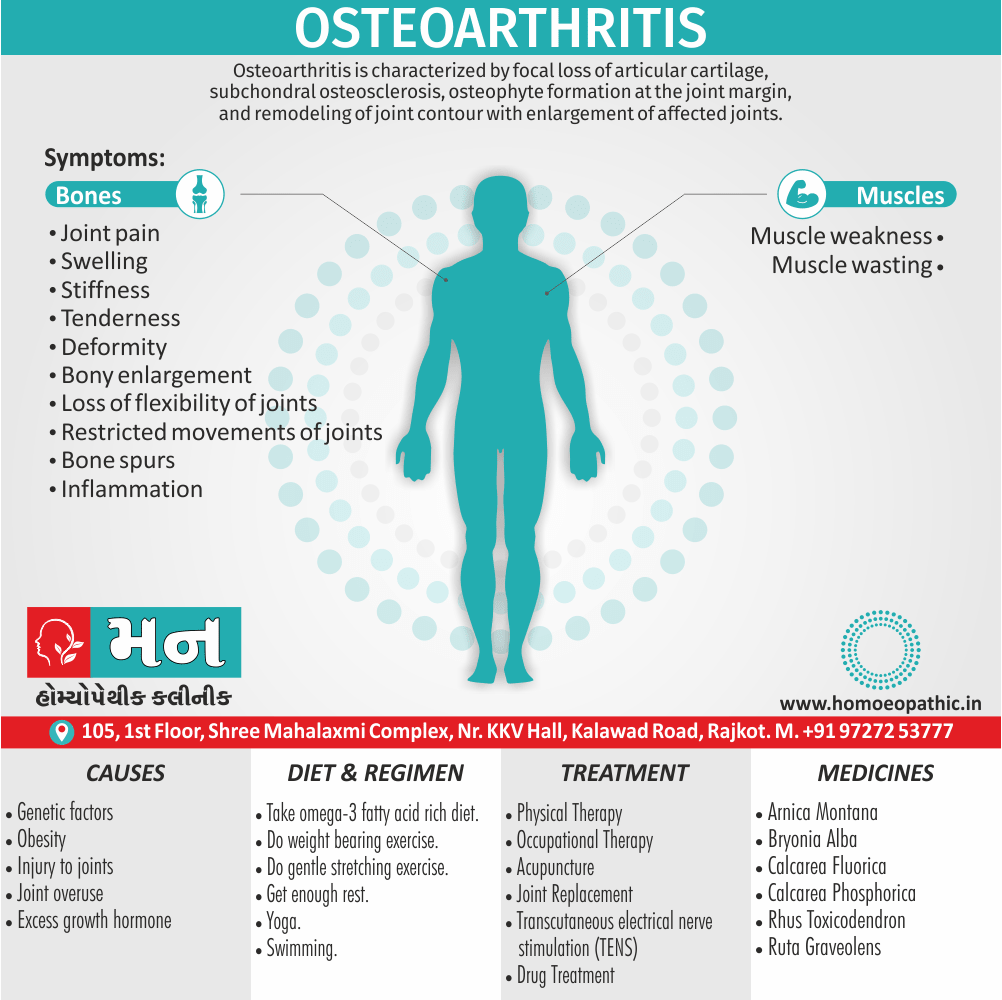
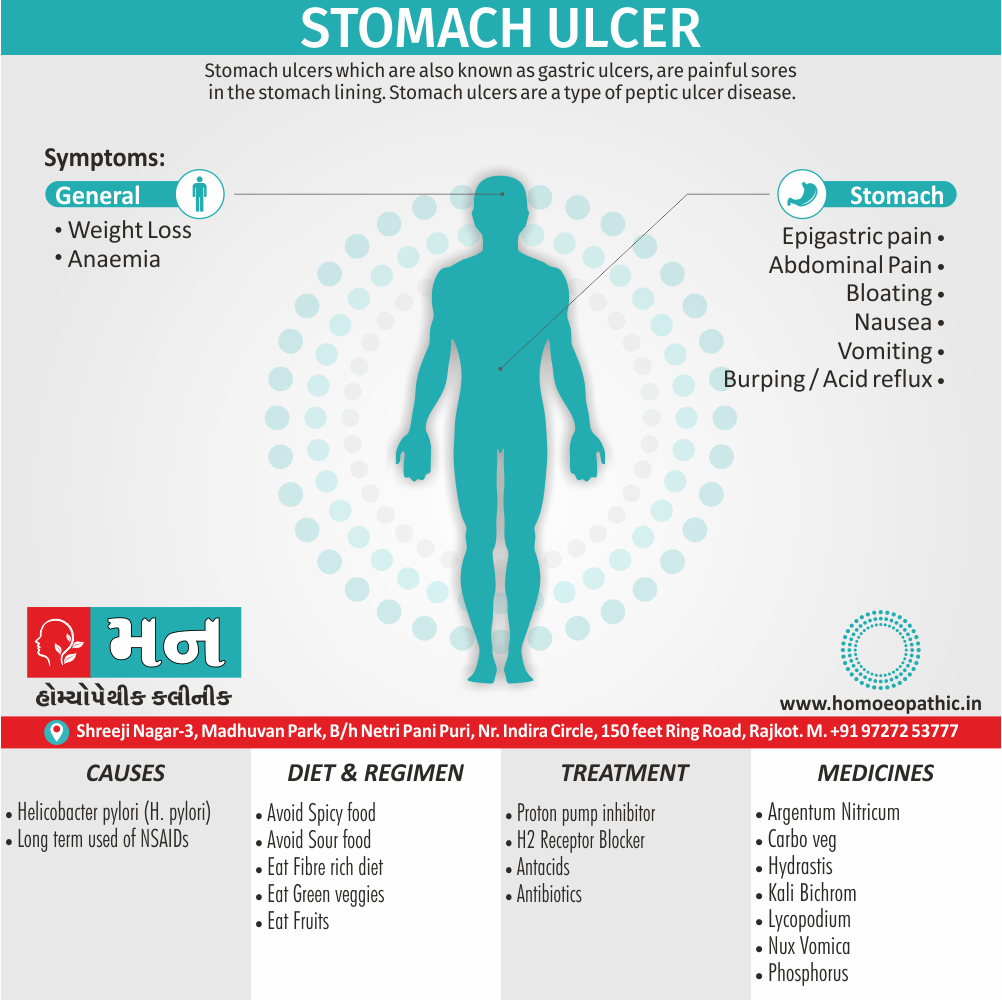
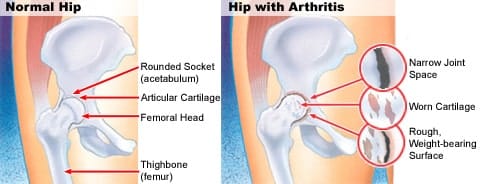
Osteoarthritis (OA) is characterized by focal loss of articular cartilage, subchondral osteosclerosis, osteophyte formation at the joint margin, and remodeling of joint contour with enlargement of affected joints. [1]
- Osteoarthritis (OA) is by far the most common form of arthritis.
- Moreover, It is strongly associate with ageing and is a major cause of pain and disability in older people.
- Inflammation can occur but is not a prominent feature.
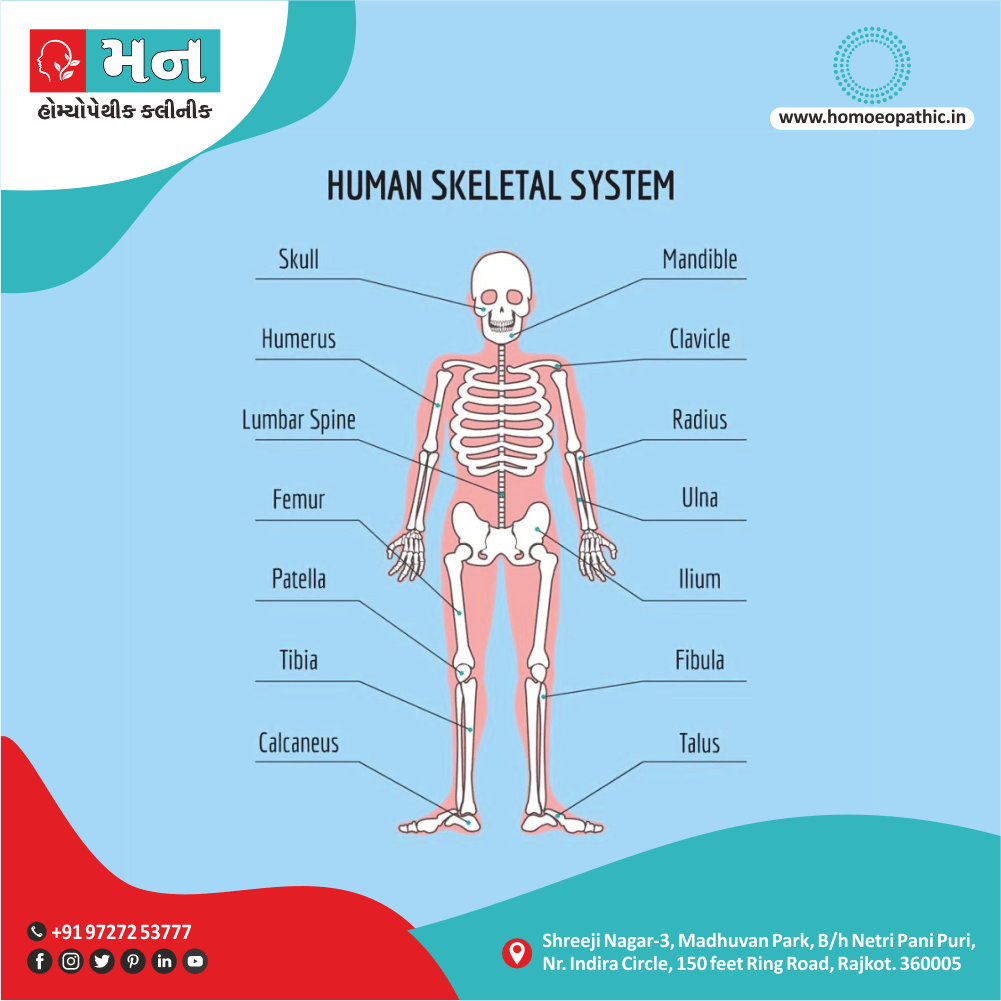
- Joint involvement in Osteoarthritis (OA) follows a characteristic distribution, mainly targeting the hips, knees, PIP (Proximal Interphalangeal Joint) & DIP (in other words, Distal Interphalangeal Joint) of the hands, neck and lumbar spine.
- The prevalence of osteoarthritis (OA) rises progressively with age and it has estimated that 45% of all people develop knee OA also 25% hip OA at some point during life.
- Although some of these patients are asymptomatic, the lifetime risk of having a total either hip or knee replacement for OA in someone aged 50 is about 11% in women and 8% in men.
- Symptoms attributable to osteoarthritis (OA) are more prevalent in women, except at the hip, where men are equally affected. [1]
- A joint is where two bones come together. Additionally; the ends of these bones are cover with protective tissue called cartilage. With OA, this cartilage breaks down, causing the bones within the joint to rub together. Besides this, This can cause pain, stiffness, and other symptoms.
- Osteoarthritis (OA) occurs most often in older people, although it can occur in adults of any age.
- All in all; Osteoarthritis (OA) is also call degenerative joint disease, degenerative arthritis, and wear-and-tear arthritis. [3]
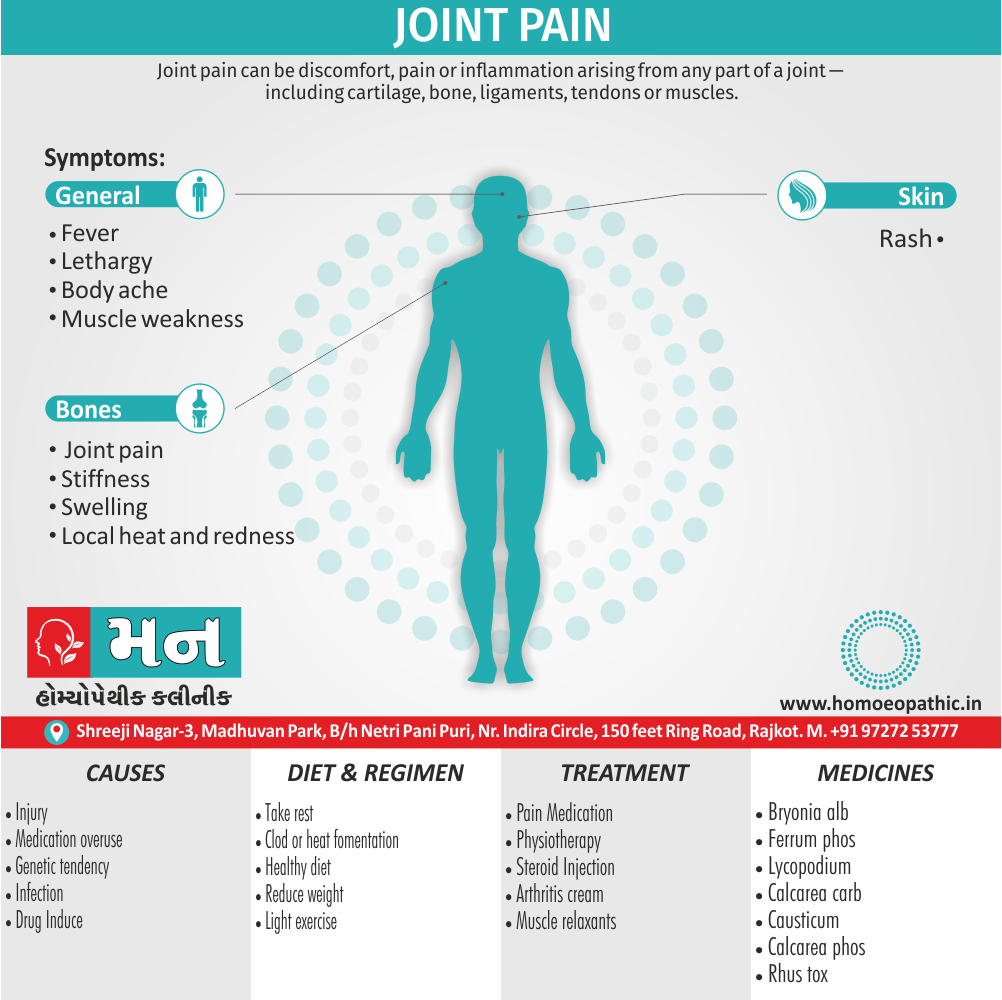
Pain:
- Insidious onset over months or years
- Either Variable or intermittent over time (‘good days, bad days’)
- Mainly related to movement and weight-bearing, relieve especially by rest
- Only brief (< 15 mins) morning stiffness also brief (< 5 mins) ‘gelling’ after rest
- Usually only one or a few joints painful
Clinical signs in Osteoarthritis (OA):
- Restricted movement due to capsular thickening, or blocking by osteophyte
- Furthermore; Palpable, sometimes audible, coarse crepitus due to rough articular surfaces
- Bony swelling around joint margins
- Deformity, usually without instability
- Either Joint-line or periarticular tenderness
- Muscle weakness also wasting
- Synovitis mild or absent
Types:
Generalised nodal OA:
Characteristics of generalised nodal osteoarthritis i.e.:

Heberden’s Nodes
- Polyarticular finger interphalangeal joint Osteoarthritis (OA)
- Heberden’s (± Bouchard’s) nodes
- Marked female preponderance
- Peak onset in middle age
- Good functional outcome for hands
- Predisposition to Osteoarthritis (OA) at other joints, especially knees
- Strong genetic predisposition
Some patients are asymptomatic whereas others develop pain, stiffness and swelling of one or more PIP joints of the hands from the age of about 40 years onward.
Gradually, these develop posterolateral swellings on each side of the extensor tendon that slowly enlarge and harden to become Heberden’s (DIP) and Bouchard’s (PIP) nodes.
Typically, each joint goes through a phase of episodic symptoms (1–5 years) while the node evolves and OA develops.
Once OA is fully establish, symptoms may subside and hand function often remains good.
Affected joints are enlarge as the result of osteophyte formation and often show characteristic lateral deviation, reflecting the asymmetric focal cartilage loss of Osteoarthritis (OA).
Involvement of the first carpometacarpal joint (CMC) is also common, leading to pain on trying to open bottles and jars and functional impairment.
Clinically, it may detect by the presence of crepitus on joint movement, and squaring of the thumb base.
Generalised nodal OA has a very strong genetic component: the daughter of an affected mother has a 1 in 3 chance of developing nodal OA herself. [1]
Knee OA:
Osteoarthritis Of Knee
Location i.e.:
OA principally targets the patellofemoral and medial tibiofemoral compartments at this site but eventually spreads to affect the whole of the joint.
It may isolate or occur as part of generalised nodal OA.
Most patients, particularly women, have bilateral and symmetrical involvement.
With men, trauma is a more important risk factor and may result in unilateral OA.
Pain i.e.:
The pain is usually localised to the anterior or medial aspect of the knee and upper tibia.
Patellofemoral pain is usually worse going up and down stairs or inclines.
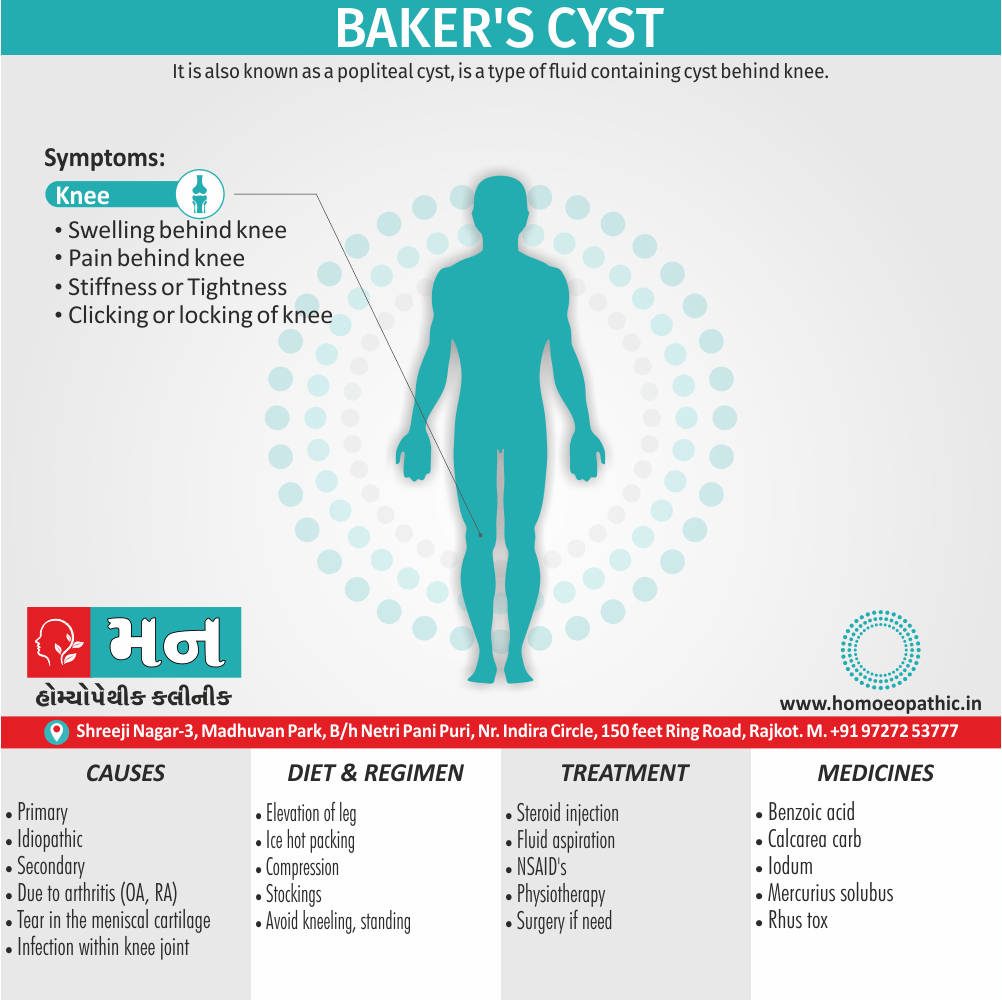
Posterior knee pain suggests the presence of a complicating popliteal cyst (Baker’s cyst).
Prolonged walking, rising from a chair, getting in or out of a car, or bending to put on shoes and socks may be difficult.
Local examination findings may include i.e.:
- A jerky, asymmetric (antalgic) gait with less time weight bearing on the painful side
- A varus, less commonly valgus, and/or fixed flexion deformity
- Joint line and/or periarticular tenderness (secondary anserine bursitis and medial ligament enthesopathy, causing tenderness of the upper medial tibia)
- Weakness and wasting of the quadriceps muscle
- Restricted flexion/extension with coarse crepitus
- Bony swelling around the joint line
Calcium pyrophosphate dihydrate (CPPD) crystal deposition in association with OA is most common at the knee. [1]
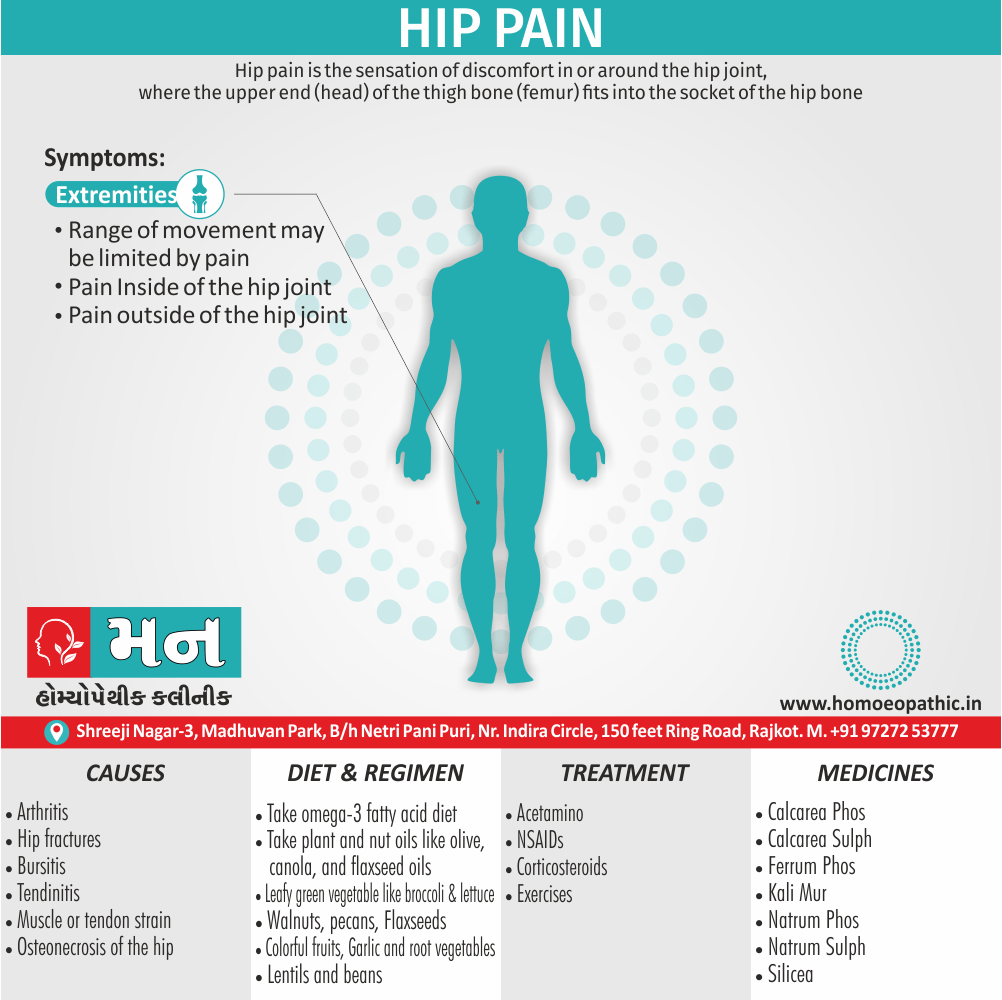
Hip OA:
Location i.e.:
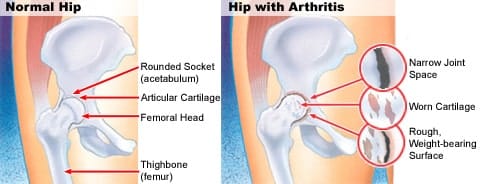
Osteoarthritis Of Hip
Hip OA most commonly targets the superior aspect of the joint.
This is often unilateral at presentation, frequently progresses with superolateral migration of the femoral head, and has a poor prognosis.
The less common central (medial) Osteoarthritis-OA shows more central cartilage loss and is largely confined to women.
It is often bilateral at presentation and may associate with generalised nodal OA.
It has a better prognosis than superior hip OA and progression to axial migration of the femoral head is uncommon.
Pain i.e.:
Hip pain is usually maximal deep in the anterior groin, with variable radiation to the buttock, anterolateral thigh, knee or shin.
Lateral hip pain, worse on lying on that side with tenderness over the greater trochanter, suggests secondary trochanteric bursitis.
Common functional difficulties are the same as for knee Osteoarthritis-OA; in addition, restricted hip abduction in women may cause pain on intercourse.
Examination may reveal i.e.:
- An antalgic gait
- Weakness and wasting of quadriceps and gluteal muscles
- Pain and restriction of internal rotation with the hip flexed the earliest and most sensitive sign of hip OA; other movements may subsequently restricted and painful
- Anterior groin tenderness just lateral to the femoral pulse
- Fixed flexion, external rotation deformity of the hip
- Ipsilateral leg shortening with severe joint attrition and superior femoral migration.
Although obesity is not a major risk factor for development of hip Osteoarthritis-OA, it is associated with more rapid progression.
Spine OA:
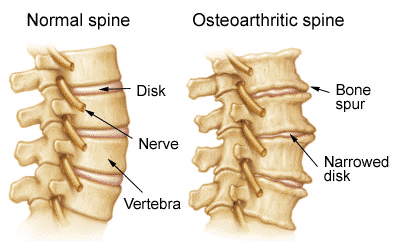
Osteoarthritis Of Spine
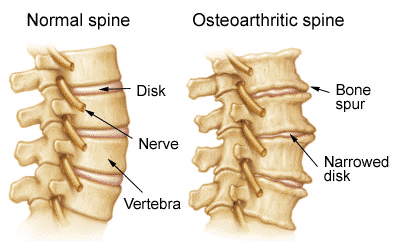
- The cervical and lumbar spine are predominantly targeted by OA, then referred to as cervical spondylosis and lumbar spondylosis, respectively.
- Spine OA may occur in isolation or as part of generalised OA.
- The typical presentation is with pain localised to the low back region or the neck, although radiation of pain to the arms, buttocks and legs may also occur due to nerve root compression.
- The pain is typically relieved by rest and worse on movement.
- On physical examination, the range of movement may be limited and loss of lumbar lordosis is typical.
- The straight leg raising test or femoral stretch test may be positive and neurological signs may be seen in the legs where there is complicating spinal stenosis or nerve root compression.
Early-onset OA:
- Unusually, typical symptoms and signs of Osteoarthritis-OA may present before the age of 45.
- In most cases, a single joint is affected and there is a clear history of previous trauma.
- However, specific causes of OA need to be considered in people with early onset disease affecting several joints, especially those not normally targeted by Osteoarthritis-OA, rare causes need to be considered.
- Kashin– Beck disease is a rare form of Osteoarthritis-OA that occurs in children, typically between the ages of 7 and 13, in some regions of China.
- The cause is unknown but suggested predisposing factors are selenium deficiency and contamination of cereals with mycotoxin producing fungi.
Causes of early-onset osteoarthritis:
Monoarticular e.g.:
- Previous trauma
- Localised instability
Pauciarticular or polyarticular e.g.:
- Juvenile idiopathic arthritis
- Metabolic or endocrine disease: for example Haemochromatosis, Ochronosis, Acromegaly
- Spondyloepiphyseal dysplasia
- Late avascular necrosis
- Neuropathic joint
- Kashin–Beck disease [1]
There are several factors that increase a person’s chances of developing osteoarthritis.
Causes of Osteoarthritis-OA:
Heredity i.e.:
- Some people have an inherited defect in one of the genes responsible for making cartilage.
- This causes defective cartilage, which leads to more rapid deterioration of joints.
- People born with joint abnormalities are more likely to develop osteoarthritis, and those born with an abnormality of the spine(such as scoliosis or curvature of the spine) are more likely to develop osteoarthritis of the spine.
Obesity i.e.:
- Obesity increases the risk for osteoarthritis of the knee, hip, and spine.
- Maintaining ideal weight or losing excess weight may help prevent osteoarthritis of these areas or decrease the rate of progression once Osteoarthritis-OA is established.
Injury i.e.:
- Injuries contribute to the development of osteoarthritis.
- For example, athletes who have knee-related injuries may be at higher risk of developing osteoarthritis of the knee.
- In addition, people who have had a severe back injury may predispose to develop osteoarthritis of the spine.
- People who have had a broken bone near a joint are prone to develop osteoarthritis in that joint.
Joint overuse i.e.:
- Overuse of certain joints increases the risk of developing osteoarthritis.
- For example, people in jobs requiring repeated bending of the knee are at increase risk for developing osteoarthritis of the knee.
Other diseases i.e.:
- People with rheumatoid arthritis, the second most common type of arthritis, are more likely to develop osteoarthritis.
- In addition, certain rare conditions, such as iron overload or excess growth hormone, increase the chance of developing Osteoarthritis-OA. [4]
There is no blood test for the diagnosis of osteoarthritis.
Blood tests are performed to exclude diseases that can cause secondary osteoarthritis, as well as to exclude other arthritis conditions that can mimic osteoarthritis.
X-rays:
- X-rays of the affected joints can use to diagnose osteoarthritis.
- The common X-ray findings of Osteoarthritis-OA include loss of joint cartilage, narrowing of the joint space between adjacent bones, and bone spur formation.
- Simple X-ray testing can also very helpful to exclude other causes of pain in a particular joint as well as assisting the decision-making as to when surgical intervention might consider.
Arthrocentesis:
- Arthrocentesis is a procedure to remove joint fluid that is often performed in a health care professional’s office.
- During arthrocentesis, a sterile needle is use to remove joint fluid for analysis.
- Joint fluid analysis is useful in excluding gout, infection, and other causes of arthritis.
- Removal of joint fluid and injection of corticosteroids into the joints during arthrocentesis can help relieve pain, swelling, and inflammation.
Arthroscopy:
- Arthroscopy is a surgical technique whereby a doctor inserts a viewing tube into the joint space.
- Abnormalities of and damage to the cartilage and ligaments can detect and sometimes repair through the arthroscope.
- If successful, patients can recover from the arthroscopic surgery much more quickly than from open joint surgery.
Finally, a careful analysis of the location, duration, and character of the joint symptoms and the appearance of the joints helps the doctor in diagnosing osteoarthritis.
Bony enlargement of the joints from spur formations is characteristic of osteoarthritis.
Therefore, the presence of Heberden’s nodes, Bouchard’s nodes, and bunions of the feet can indicate to the doctor a diagnosis of osteoarthritis. [5]
Management of Osteoarthritis (OA):
OA treatment is centered upon symptom management.
The type of treatment that will help you the most will largely be determined by the severity of your symptoms and their location.
Often, lifestyle changes, over-the-counter (OTC) medication, and home remedies will be enough to provide you with relief from pain, stiffness, and swelling.
At-home treatments and lifestyle changes for Osteoarthritis-OA include:
Exercise i.e.:
- Physical activity strengthens the muscles around your joints and may help relieve stiffness.
- Aim for at least 20 to 30 minutes of physical movement, at least every other day.
- Choose gentle, low-impact activities, such as walking or swimming.
- Tai chi and yoga can also improve joint flexibility and help with pain management.
- Gentle stretching exercises can be very helpful for people with Osteoarthritis-OA, especially if you have stiffness or pain in your knees, hips, or back.
- Stretching can help improve mobility and range of motion.
Weight loss i.e.:
- Being higher-weight person can put strain on your joints and cause pain.
- Shedding excess pounds helps relieve this pressure and reduces pain.
- A healthy weight can also lower your risk of other health problems, such as diabetes and heart disease.
Adequate sleep i.e.:
- Resting your muscles can reduce swelling and inflammation.
- Be kind to yourself and don’t overdo it.
- Getting enough sleep at night can also help you to manage pain more effectively.
Heat and cold therapy i.e.:
- You can experiment with heat or cold therapy to relieve muscle pain and stiffness.
- Apply a cold or hot compress to sore joints for 15 to 20 minutes several times a day.
These practices can help take the edge off of your symptoms and improve your quality of life.
Medications of Osteoarthritis-OA:
There are a number of different types of Osteoarthritis-OA medications that can help provide relief from pain or swelling.
Oral analgesics i.e.:
- Tylenol (acetaminophen) and other pain relievers reduce pain but not swelling.
Topical analgesics i.e.:
- These OTC products are available as creams, gels, and patches.
- They help to numb the joint area and can provide pain relief, especially for mild arthritis pain.
NSAIDs (nonsteroidal anti-inflammatory drugs) i.e.:
- NSAIDs such as Advil (ibuprofen) and Aleve (naproxen) reduce swelling as well as pain.
Cymbalta i.e.:
- Your doctor may prescribe the antidepressant Cymbalta (duloxetine) for you off-label to help provide osteoarthritis(OA) pain relief.
Corticosteroids i.e.:
- These prescription medications are available in oral form.
- They may also be given by injection directly into a joint.
Natural treatments:
Alternative treatments and supplements may help to relieve symptoms such as inflammation and joint pain.
Some supplements or herbs that may help include:
- Fish oil
- Green tea
- Ginger
- Glucosamine
Other alternative treatment options include:
- Acupuncture
- Physical therapy
- Massage therapy
Other remedies can range from taking Epsom salt baths to using hot or cold compresses.
Diet:
There’s no downside to eating healthy, but if you have Osteoarthritis-OA, diet and nutrition are especially important.
Some types of Osteoarthritis-OA, such as osteoarthritis of the knee, respond positively to a diet high in flavonoids, which are nutrients found in fruits and vegetables.
Also, the antioxidants found in many fruits and vegetables may also help combat the free radicals produced by inflammation. Free radicals are molecules that can cause cell damage.
A high-quality diet may help provide relief from osteoarthritis (OA) symptoms by reducing inflammation and swelling.
Eating foods high in the following can be highly beneficial:
- Vitamin C
- Vitamin D
- Beta-carotene
- Omega-3 fatty acids
Increasing your intake of foods with anti-inflammatory properties will help, too. [3]
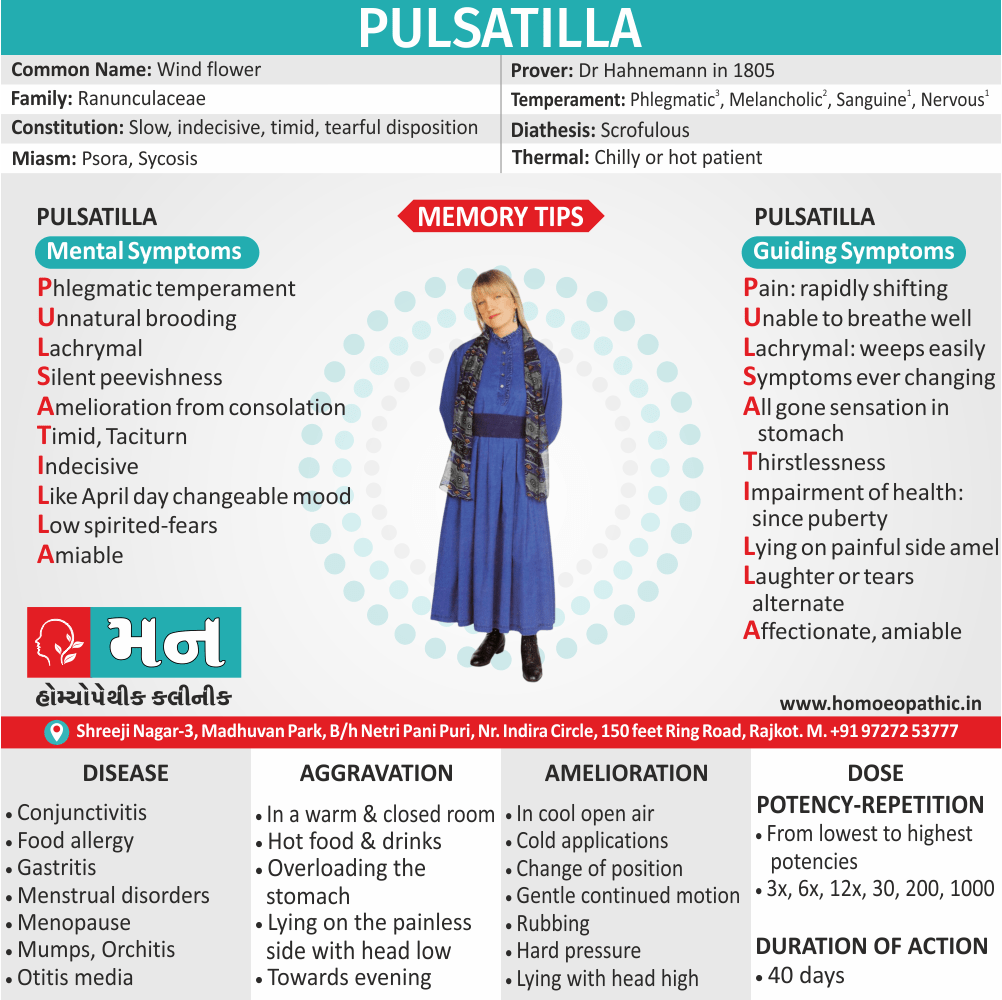
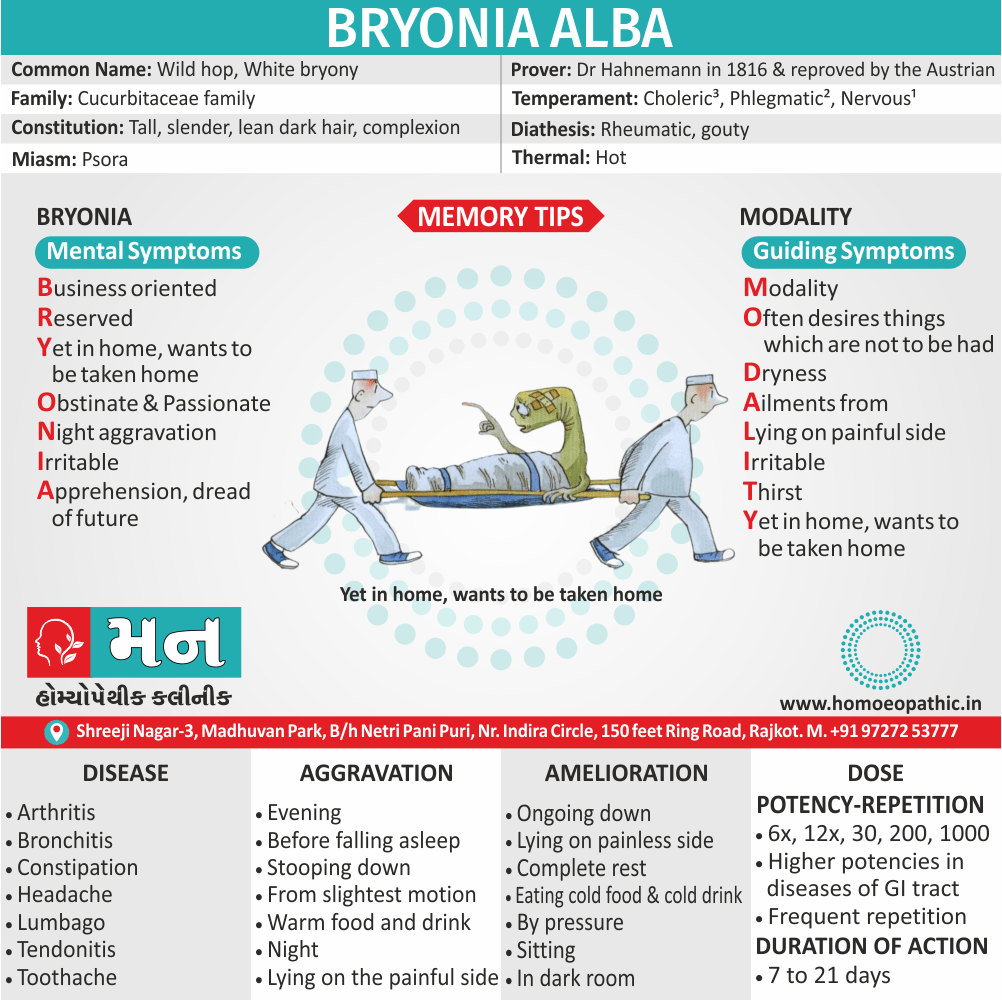
Bryonia Alba:
- Excellent remedy which is useful in treatment of osteoarthritis, pain with inflammation which is aggravated by movement on the other hand relieved by moderate pressure and rest.
- There is inflammation of joints which are hot also swollen.
Rhus Toxicodendron:
- Recurring attacks due to getting chilled.
- Rheumatism caused by damp weather and worse in damp climate; there is restlessness and the pains are worse on first motion, better by continued motion.
Kali Carb:
- Pains stitching, stabbing and burning character relieved temporarily by cold application and not by rest or motion.
- The patient shrieks on account of pain.
- Backache accompanied by great weakness.
Arnica:
- Generally, Chronic arthritis with a feeling of bruised soreness can indicate a need for this remedy.
- Pain is worse specifically from touch, and may occur in joints that were injured in the past.
Ruta graveolens:
- Arthritis with a feeling of great stiffness and lameness, worse from cold and damp, and worse from exertion often is relieved by this remedy.
- Tendons and the capsules of the joints may be affected.
- Besides this; Arthritis may have developed after overuse, from repeated wear and tear.
Kalmia latifolia:
- Intense arthritic pain that appears quite suddenly may indicate this medicine especially when the problems start in higher joints and extend to lower ones.
- Pain and inflammation often start in the shoulder, moving to the elbow, wrist and hand.
- The knees are also frequently affected.
- Discomfort is worse from motion and often worse at night.
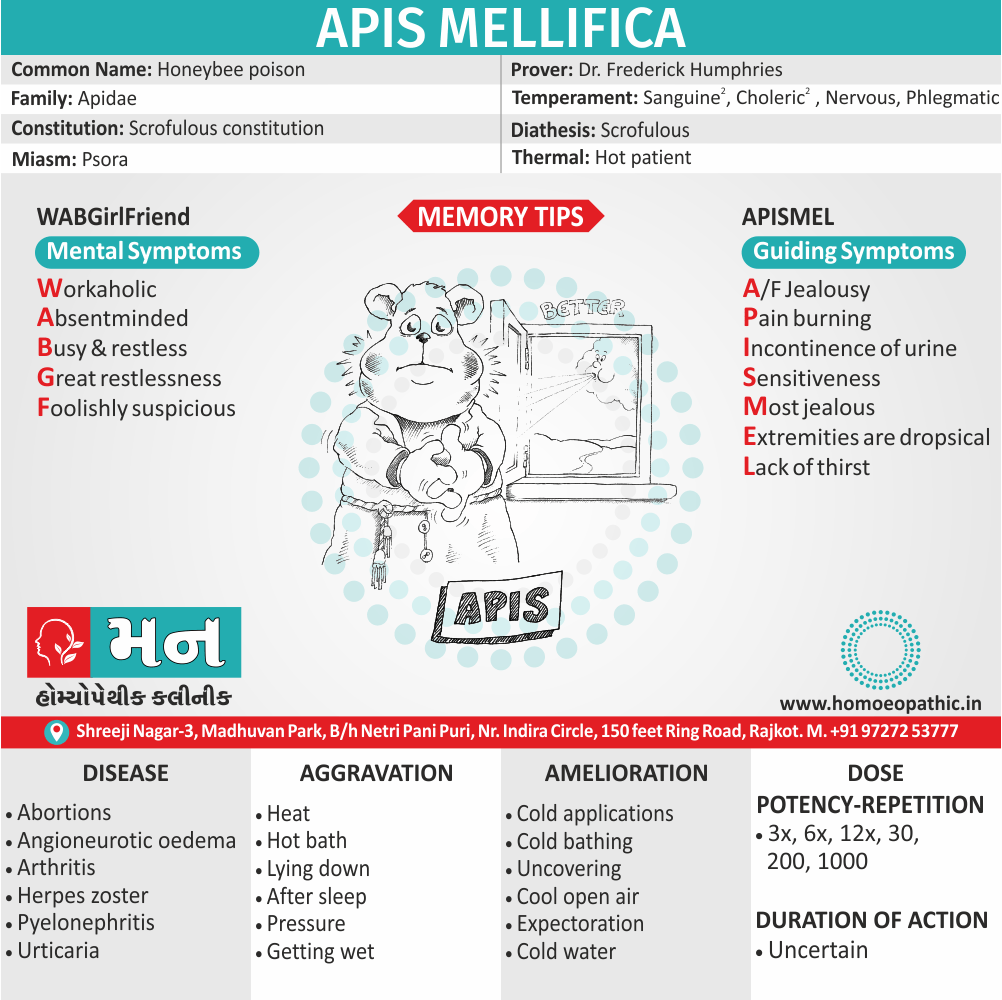
Apis mellifica:
- This remedy can be helpful in acute conditions with redness, tenderness, also swelling.
- Joints feel hot and have stinging pain.
- The hands and knees are often affected.
- Warmth can aggravate the symptoms and cool applications bring relief.
Calcarea fluorica:
- This medicine is often indicated for arthritic pains that are improved especially by heat and motion.
- Joints become enlarged also hard, and nodosities or bone spurs may develop.
- Arthritis after chronic injury to joints often responds to Calcarea fluorica.
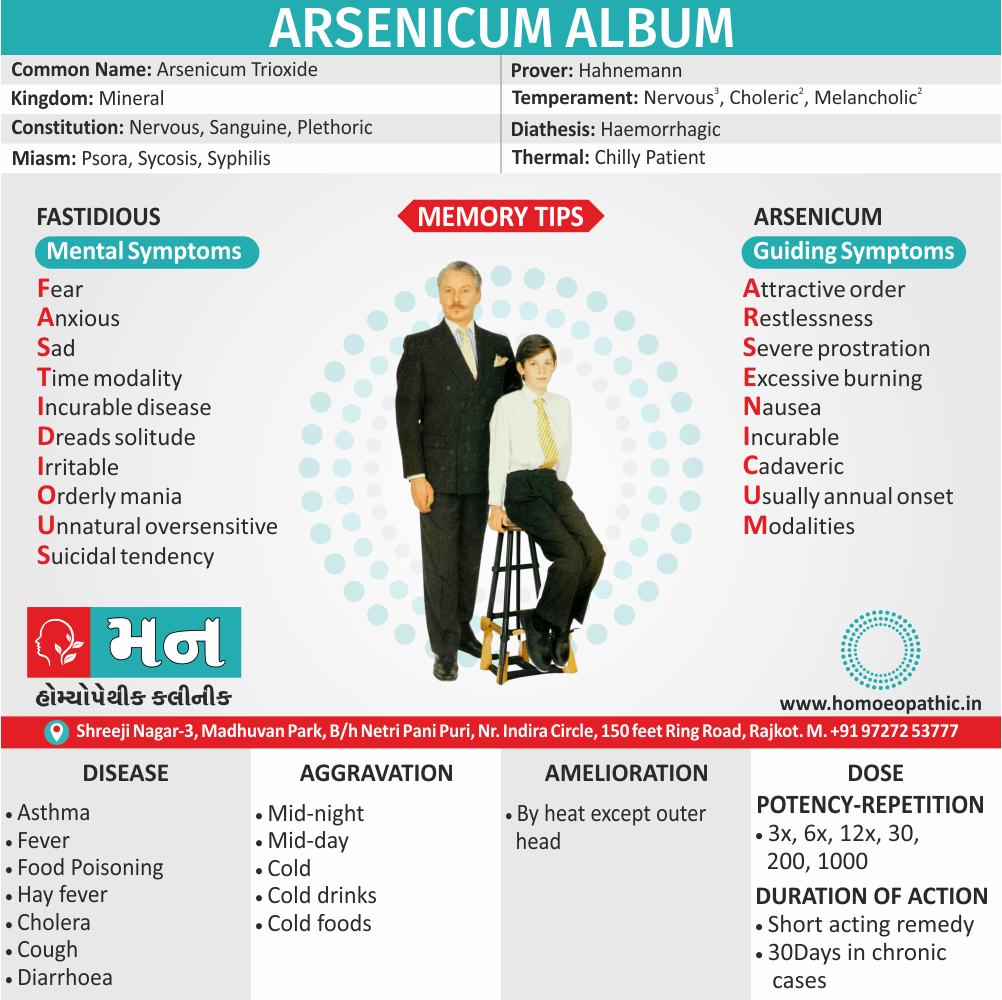
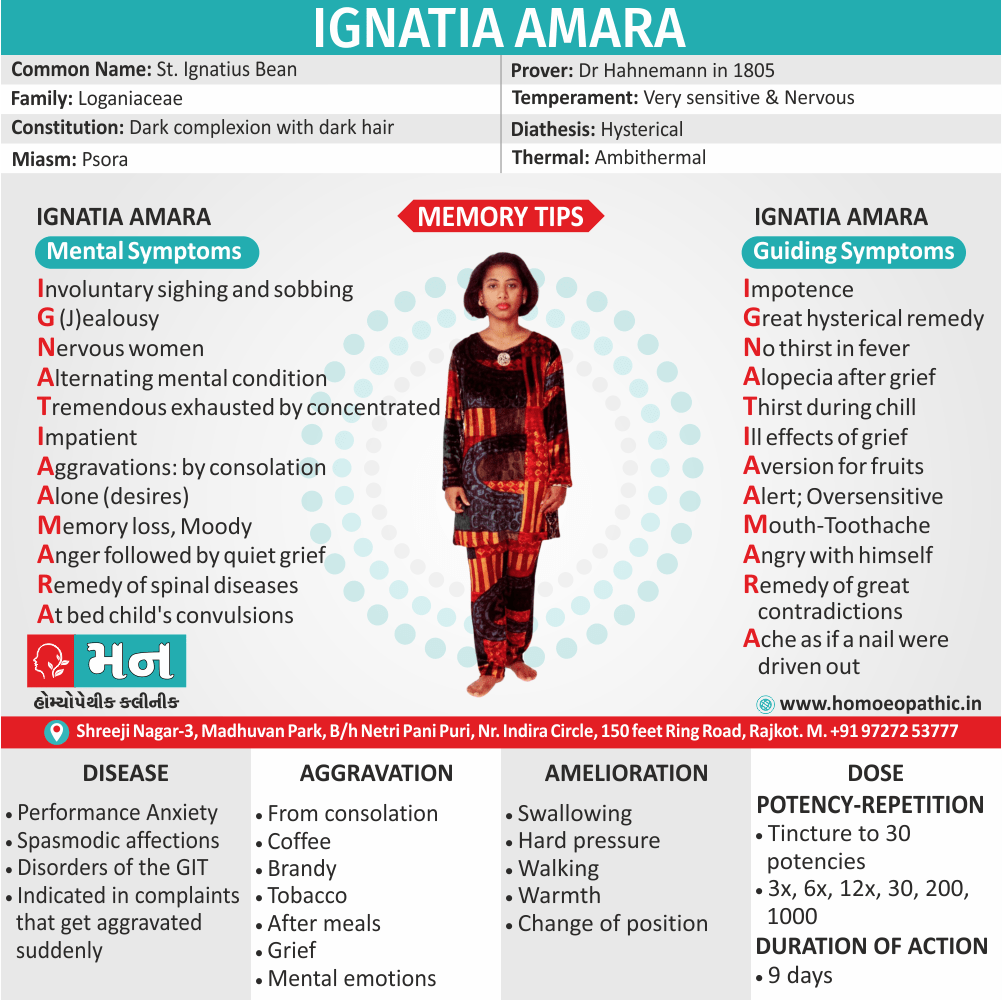
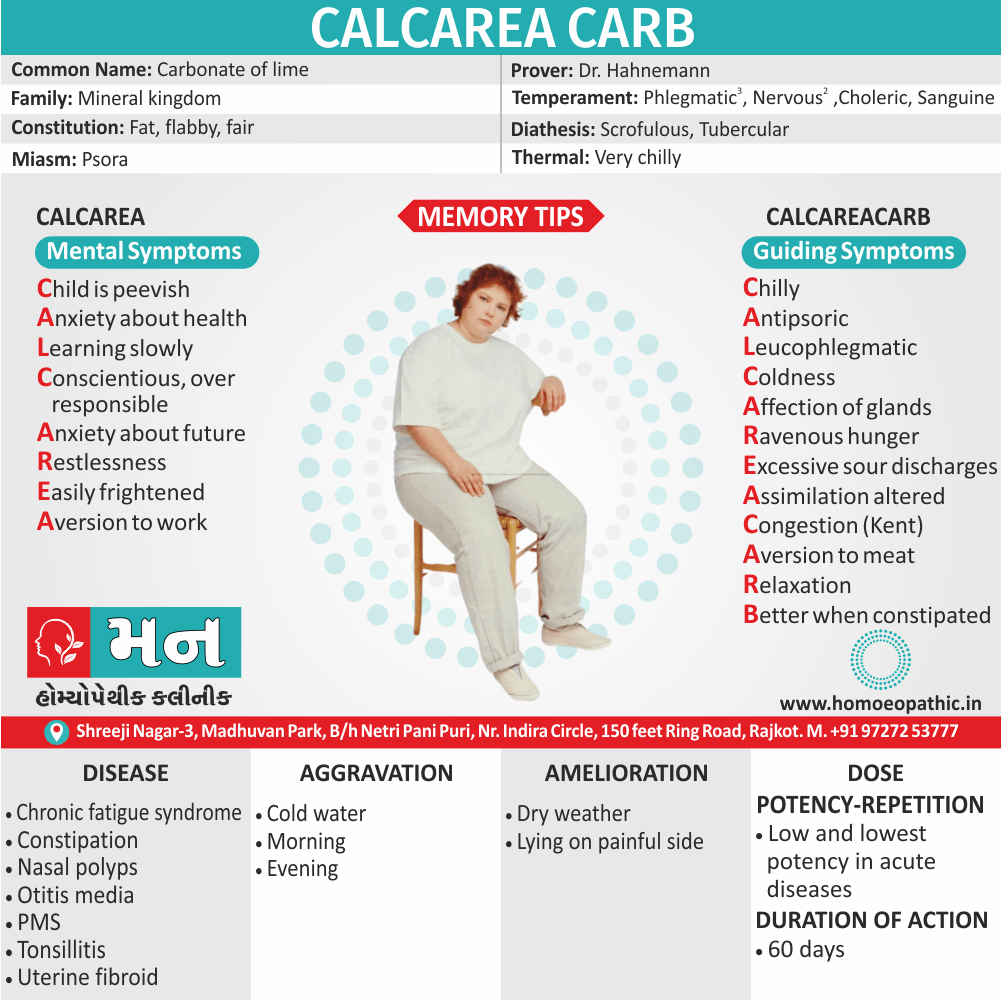
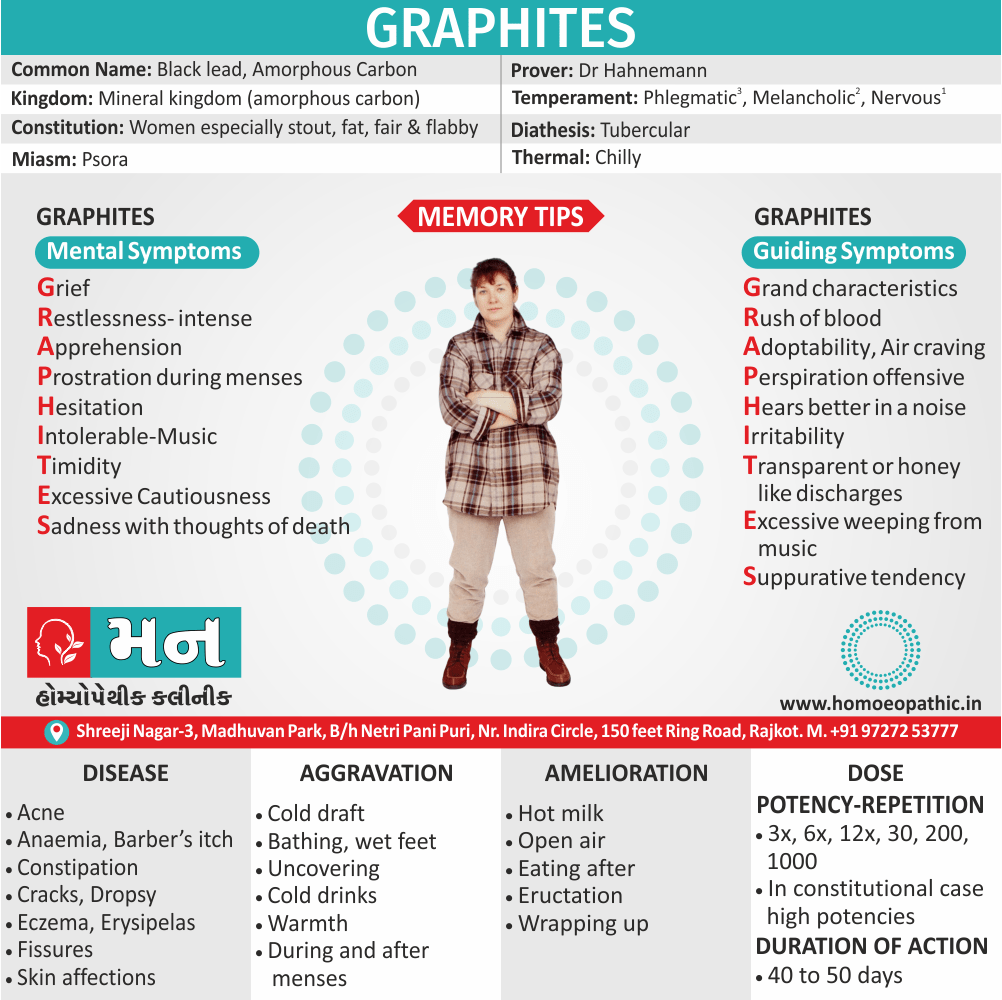
Calcarea carbonica:
- This remedy is often useful for arthritis in a person who is flabby or higher-weight person , and easily tired by exertion.
- Inflammation and soreness are worse from cold and dampness, and weakness or cramping in the extremities are often seen.
- Problems often focus on the knees when Calcarea is needed.
Sticta Pulmonaria:
- Rheumatism of right shoulder blade or joint, wrist joint, ankle joint and knee joint.
- It also reduces fluid in the joints. [6]
Frequently Asked Questions
What is Osteoarthritis?
Osteoarthritis (OA) is characterized by focal loss of articular cartilage, subchondral osteosclerosis, osteophyte formation at the joint margin, and remodeling of joint contour with enlargement of affected joints.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Osteoarthritis?
- Bryonia Alba
- Rhus Tox
- Kali Carb
- Arnica
- Ruta graveolens
- Kalmia latifolia
- Apis mellifica
- Calcarea fluorica
- Calcarea carbonica
- Sticta Pulmonaria
What causes Osteoarthritis?
- Heredity
- Obesity
- Injury
- Joint overuse
- Other diseases
What are the symptoms of Osteoarthritis?
- Pain: Insidious onset, intermittent, morning stiffness
- Restricted movement
- Palpable, sometimes audible, coarse crepitus
- Bony swelling around joint margins
- Deformity, usually without instability
- Either Joint-line or periarticular tenderness
- Muscle weakness also wasting
- Synovitis mild or absent
Give the types of Osteoarthritis?
- Generalised nodal OA
- Knee OA
- Hip OA
- Spine OA
- Early-onset OA
-
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 25
- https://www.mayoclinic.org/diseases-conditions/osteoarthritis/symptoms-causes/syc-20351925
- https://www.healthline.com/health/osteoarthritis#osteoarthritis-symptoms
- https://www.webmd.com/osteoarthritis/guide/osteoarthritis-basics#1
- https://www.medicinenet.com/osteoarthritis/article.htm#how_do_health_care_professionals_diagnose_osteoarthritis
- http://homeopathyclinic.co.in/10-best-homeopathic-medicines-treatment-osteoarthritis/
Definition: Osteoarthritis (OA) is characterized by focal loss of articular cartilage, subchondral osteosclerosis, osteophyte formation at the joint margin, and remodeling of joint contour with enlargement of affected joints. [1]
Overview
Epidemiology
Causes
Risk Factors
Pathogenesis
Pathophysiology
Types
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Dont’s
Terminology
References
FAQ
Also Search As
Overview
- Osteoarthritis (OA) is by far the most common form of arthritis.
- Moreover, It is strongly associate with ageing and is a major cause of pain and disability in older people.
- Inflammation can occur but is not a prominent feature.
- Joint involvement in Osteoarthritis (OA) follows a characteristic distribution, mainly targeting the hips, knees, PIP (Proximal Interphalangeal Joint) & DIP (in other words, Distal Interphalangeal Joint) of the hands, neck and lumbar spine.
- The prevalence of osteoarthritis (OA) rises progressively with age and it has estimated that 45% of all people develop knee OA also 25% hip OA at some point during life.
- Although some of these patients are asymptomatic, the lifetime risk of having a total either hip or knee replacement for OA in someone aged 50 is about 11% in women and 8% in men.
- Symptoms attributable to osteoarthritis (OA) are more prevalent in women, except at the hip, where men are equally affected. [1]
- A joint is where two bones come together. Additionally; the ends of these bones are cover with protective tissue called cartilage. With OA, this cartilage breaks down, causing the bones within the joint to rub together. Besides this, This can cause pain, stiffness, and other symptoms.
- Osteoarthritis (OA) occurs most often in older people, although it can occur in adults of any age.
- All in all; Osteoarthritis (OA) is also call degenerative joint disease, degenerative arthritis, and wear-and-tear arthritis. [3]
Epidemiology
Indian epidemiology then other
Causes
There are several factors that increase a person’s chances of developing osteoarthritis.
Causes of Osteoarthritis-OA:
Heredity i.e.:
- Some people have an inherited defect in one of the genes responsible for making cartilage.
- This causes defective cartilage, which leads to more rapid deterioration of joints.
- People born with joint abnormalities are more likely to develop osteoarthritis, and those born with an abnormality of the spine(such as scoliosis or curvature of the spine) are more likely to develop osteoarthritis of the spine.
Obesity i.e.:
- Obesity increases the risk for osteoarthritis of the knee, hip, and spine.
- Maintaining ideal weight or losing excess weight may help prevent osteoarthritis of these areas or decrease the rate of progression once Osteoarthritis-OA is established.
Injury i.e.:
- Injuries contribute to the development of osteoarthritis.
- For example, athletes who have knee-related injuries may be at higher risk of developing osteoarthritis of the knee.
- In addition, people who have had a severe back injury may predispose to develop osteoarthritis of the spine.
- People who have had a broken bone near a joint are prone to develop osteoarthritis in that joint.
Joint overuse i.e.:
- Overuse of certain joints increases the risk of developing osteoarthritis.
- For example, people in jobs requiring repeated bending of the knee are at increase risk for developing osteoarthritis of the knee.
Other diseases i.e.:
- People with rheumatoid arthritis, the second most common type of arthritis, are more likely to develop osteoarthritis.
- In addition, certain rare conditions, such as iron overload or excess growth hormone, increase the chance of developing Osteoarthritis-OA. [4]
Risk Factors
Risk factors are things that make you more likely to develop a disease in the first place.
Pathogenesis
Pathogenesis refers to the development of a disease. It’s the story of how a disease gets started and progresses.
This is the entire journey of a disease, encompassing the cause but going beyond it.
Pathophysiology
Pathophysiology, on the other hand, focuses on the functional changes that occur in the body due to the disease. It explains how the disease disrupts normal physiological processes and how this disruption leads to the signs and symptoms we see.
Imagine a car accident. Pathogenesis would be like understanding how the accident happened – what caused it, the sequence of events (e.g., one car ran a red light, then hit another car). Pathophysiology would be like understanding the damage caused by the accident – the bent fenders, deployed airbags, and any injuries to the passengers.
In simpler terms, pathogenesis is about the "why" of a disease, while pathophysiology is about the "how" of the disease’s effects.
Types
AAA
Clinical Features
Tab Content
Sign & Symptoms
Pain:
- Insidious onset over months or years
- Either Variable or intermittent over time (‘good days, bad days’)
- Mainly related to movement and weight-bearing, relieve especially by rest
- Only brief (< 15 mins) morning stiffness also brief (< 5 mins) ‘gelling’ after rest
- Usually only one or a few joints painful
Clinical signs in Osteoarthritis (OA):
- Restricted movement due to capsular thickening, or blocking by osteophyte
- Furthermore; Palpable, sometimes audible, coarse crepitus due to rough articular surfaces
- Bony swelling around joint margins
- Deformity, usually without instability
- Either Joint-line or periarticular tenderness
- Muscle weakness also wasting
- Synovitis mild or absent
Types:
Generalised nodal OA:
Characteristics of generalised nodal osteoarthritis i.e.:

Heberden’s Nodes
- Polyarticular finger interphalangeal joint Osteoarthritis (OA)
- Heberden’s (± Bouchard’s) nodes
- Marked female preponderance
- Peak onset in middle age
- Good functional outcome for hands
- Predisposition to Osteoarthritis (OA) at other joints, especially knees
- Strong genetic predisposition
Some patients are asymptomatic whereas others develop pain, stiffness and swelling of one or more PIP joints of the hands from the age of about 40 years onward.
Gradually, these develop posterolateral swellings on each side of the extensor tendon that slowly enlarge and harden to become Heberden’s (DIP) and Bouchard’s (PIP) nodes.
Typically, each joint goes through a phase of episodic symptoms (1–5 years) while the node evolves and OA develops.
Once OA is fully establish, symptoms may subside and hand function often remains good.
Affected joints are enlarge as the result of osteophyte formation and often show characteristic lateral deviation, reflecting the asymmetric focal cartilage loss of Osteoarthritis (OA).
Involvement of the first carpometacarpal joint (CMC) is also common, leading to pain on trying to open bottles and jars and functional impairment.
Clinically, it may detect by the presence of crepitus on joint movement, and squaring of the thumb base.
Generalised nodal OA has a very strong genetic component: the daughter of an affected mother has a 1 in 3 chance of developing nodal OA herself. [1]
Knee OA:
Osteoarthritis Of Knee
Location i.e.:
OA principally targets the patellofemoral and medial tibiofemoral compartments at this site but eventually spreads to affect the whole of the joint.
It may isolate or occur as part of generalised nodal OA.
Most patients, particularly women, have bilateral and symmetrical involvement.
With men, trauma is a more important risk factor and may result in unilateral OA.
Pain i.e.:
The pain is usually localised to the anterior or medial aspect of the knee and upper tibia.
Patellofemoral pain is usually worse going up and down stairs or inclines.
Posterior knee pain suggests the presence of a complicating popliteal cyst (Baker’s cyst).
Prolonged walking, rising from a chair, getting in or out of a car, or bending to put on shoes and socks may be difficult.
Local examination findings may include i.e.:
- A jerky, asymmetric (antalgic) gait with less time weight bearing on the painful side
- A varus, less commonly valgus, and/or fixed flexion deformity
- Joint line and/or periarticular tenderness (secondary anserine bursitis and medial ligament enthesopathy, causing tenderness of the upper medial tibia)
- Weakness and wasting of the quadriceps muscle
- Restricted flexion/extension with coarse crepitus
- Bony swelling around the joint line
Calcium pyrophosphate dihydrate (CPPD) crystal deposition in association with OA is most common at the knee. [1]
Hip OA:
Location i.e.:
Osteoarthritis Of Hip
Hip OA most commonly targets the superior aspect of the joint.
This is often unilateral at presentation, frequently progresses with superolateral migration of the femoral head, and has a poor prognosis.
The less common central (medial) Osteoarthritis-OA shows more central cartilage loss and is largely confined to women.
It is often bilateral at presentation and may associate with generalised nodal OA.
It has a better prognosis than superior hip OA and progression to axial migration of the femoral head is uncommon.
Pain i.e.:
Hip pain is usually maximal deep in the anterior groin, with variable radiation to the buttock, anterolateral thigh, knee or shin.
Lateral hip pain, worse on lying on that side with tenderness over the greater trochanter, suggests secondary trochanteric bursitis.
Common functional difficulties are the same as for knee Osteoarthritis-OA; in addition, restricted hip abduction in women may cause pain on intercourse.
Examination may reveal i.e.:
- An antalgic gait
- Weakness and wasting of quadriceps and gluteal muscles
- Pain and restriction of internal rotation with the hip flexed the earliest and most sensitive sign of hip OA; other movements may subsequently restricted and painful
- Anterior groin tenderness just lateral to the femoral pulse
- Fixed flexion, external rotation deformity of the hip
- Ipsilateral leg shortening with severe joint attrition and superior femoral migration.
Although obesity is not a major risk factor for development of hip Osteoarthritis-OA, it is associated with more rapid progression.
Spine OA:
Osteoarthritis Of Spine
- The cervical and lumbar spine are predominantly targeted by OA, then referred to as cervical spondylosis and lumbar spondylosis, respectively.
- Spine OA may occur in isolation or as part of generalised OA.
- The typical presentation is with pain localised to the low back region or the neck, although radiation of pain to the arms, buttocks and legs may also occur due to nerve root compression.
- The pain is typically relieved by rest and worse on movement.
- On physical examination, the range of movement may be limited and loss of lumbar lordosis is typical.
- The straight leg raising test or femoral stretch test may be positive and neurological signs may be seen in the legs where there is complicating spinal stenosis or nerve root compression.
Early-onset OA:
- Unusually, typical symptoms and signs of Osteoarthritis-OA may present before the age of 45.
- In most cases, a single joint is affected and there is a clear history of previous trauma.
- However, specific causes of OA need to be considered in people with early onset disease affecting several joints, especially those not normally targeted by Osteoarthritis-OA, rare causes need to be considered.
- Kashin– Beck disease is a rare form of Osteoarthritis-OA that occurs in children, typically between the ages of 7 and 13, in some regions of China.
- The cause is unknown but suggested predisposing factors are selenium deficiency and contamination of cereals with mycotoxin producing fungi.
Causes of early-onset osteoarthritis:
Monoarticular e.g.:
- Previous trauma
- Localised instability
Pauciarticular or polyarticular e.g.:
- Juvenile idiopathic arthritis
- Metabolic or endocrine disease: for example Haemochromatosis, Ochronosis, Acromegaly
- Spondyloepiphyseal dysplasia
- Late avascular necrosis
- Neuropathic joint
- Kashin–Beck disease [1]
Clinical Examination
Tab Content
Diagnosis
There is no blood test for the diagnosis of osteoarthritis.
Blood tests are performed to exclude diseases that can cause secondary osteoarthritis, as well as to exclude other arthritis conditions that can mimic osteoarthritis.
X-rays:
- X-rays of the affected joints can use to diagnose osteoarthritis.
- The common X-ray findings of Osteoarthritis-OA include loss of joint cartilage, narrowing of the joint space between adjacent bones, and bone spur formation.
- Simple X-ray testing can also very helpful to exclude other causes of pain in a particular joint as well as assisting the decision-making as to when surgical intervention might consider.
Arthrocentesis:
- Arthrocentesis is a procedure to remove joint fluid that is often performed in a health care professional’s office.
- During arthrocentesis, a sterile needle is use to remove joint fluid for analysis.
- Joint fluid analysis is useful in excluding gout, infection, and other causes of arthritis.
- Removal of joint fluid and injection of corticosteroids into the joints during arthrocentesis can help relieve pain, swelling, and inflammation.
Arthroscopy:
- Arthroscopy is a surgical technique whereby a doctor inserts a viewing tube into the joint space.
- Abnormalities of and damage to the cartilage and ligaments can detect and sometimes repair through the arthroscope.
- If successful, patients can recover from the arthroscopic surgery much more quickly than from open joint surgery.
Finally, a careful analysis of the location, duration, and character of the joint symptoms and the appearance of the joints helps the doctor in diagnosing osteoarthritis.
Bony enlargement of the joints from spur formations is characteristic of osteoarthritis.
Therefore, the presence of Heberden’s nodes, Bouchard’s nodes, and bunions of the feet can indicate to the doctor a diagnosis of osteoarthritis. [5]
Differential Diagnosis
Complications
Complications are what happen after you have a disease. They are the negative consequences of the disease process.
Investigations
Tab Content
Treatment
Management of Osteoarthritis (OA):
OA treatment is centered upon symptom management.
The type of treatment that will help you the most will largely be determined by the severity of your symptoms and their location.
Often, lifestyle changes, over-the-counter (OTC) medication, and home remedies will be enough to provide you with relief from pain, stiffness, and swelling.
At-home treatments and lifestyle changes for Osteoarthritis-OA include:
Exercise i.e.:
- Physical activity strengthens the muscles around your joints and may help relieve stiffness.
- Aim for at least 20 to 30 minutes of physical movement, at least every other day.
- Choose gentle, low-impact activities, such as walking or swimming.
- Tai chi and yoga can also improve joint flexibility and help with pain management.
- Gentle stretching exercises can be very helpful for people with Osteoarthritis-OA, especially if you have stiffness or pain in your knees, hips, or back.
- Stretching can help improve mobility and range of motion.
Weight loss i.e.:
- Being higher-weight person can put strain on your joints and cause pain.
- Shedding excess pounds helps relieve this pressure and reduces pain.
- A healthy weight can also lower your risk of other health problems, such as diabetes and heart disease.
Adequate sleep i.e.:
- Resting your muscles can reduce swelling and inflammation.
- Be kind to yourself and don’t overdo it.
- Getting enough sleep at night can also help you to manage pain more effectively.
Heat and cold therapy i.e.:
- You can experiment with heat or cold therapy to relieve muscle pain and stiffness.
- Apply a cold or hot compress to sore joints for 15 to 20 minutes several times a day.
These practices can help take the edge off of your symptoms and improve your quality of life.
Medications of Osteoarthritis-OA:
There are a number of different types of Osteoarthritis-OA medications that can help provide relief from pain or swelling.
Oral analgesics i.e.:
- Tylenol (acetaminophen) and other pain relievers reduce pain but not swelling.
Topical analgesics i.e.:
- These OTC products are available as creams, gels, and patches.
- They help to numb the joint area and can provide pain relief, especially for mild arthritis pain.
NSAIDs (nonsteroidal anti-inflammatory drugs) i.e.:
- NSAIDs such as Advil (ibuprofen) and Aleve (naproxen) reduce swelling as well as pain.
Cymbalta i.e.:
- Your doctor may prescribe the antidepressant Cymbalta (duloxetine) for you off-label to help provide osteoarthritis(OA) pain relief.
Corticosteroids i.e.:
- These prescription medications are available in oral form.
- They may also be given by injection directly into a joint.
Natural treatments:
Alternative treatments and supplements may help to relieve symptoms such as inflammation and joint pain.
Some supplements or herbs that may help include:
- Fish oil
- Green tea
- Ginger
- Glucosamine
Other alternative treatment options include:
- Acupuncture
- Physical therapy
- Massage therapy
Other remedies can range from taking Epsom salt baths to using hot or cold compresses.
Diet:
There’s no downside to eating healthy, but if you have Osteoarthritis-OA, diet and nutrition are especially important.
Some types of Osteoarthritis-OA, such as osteoarthritis of the knee, respond positively to a diet high in flavonoids, which are nutrients found in fruits and vegetables.
Also, the antioxidants found in many fruits and vegetables may also help combat the free radicals produced by inflammation. Free radicals are molecules that can cause cell damage.
A high-quality diet may help provide relief from osteoarthritis (OA) symptoms by reducing inflammation and swelling.
Eating foods high in the following can be highly beneficial:
- Vitamin C
- Vitamin D
- Beta-carotene
- Omega-3 fatty acids
Increasing your intake of foods with anti-inflammatory properties will help, too. [3]
Prevention
Tab Content
Homeopathic Treatment
Bryonia Alba:
- Excellent remedy which is useful in treatment of osteoarthritis, pain with inflammation which is aggravated by movement on the other hand relieved by moderate pressure and rest.
- There is inflammation of joints which are hot also swollen.
Rhus Toxicodendron:
- Recurring attacks due to getting chilled.
- Rheumatism caused by damp weather and worse in damp climate; there is restlessness and the pains are worse on first motion, better by continued motion.
Kali Carb:
- Pains stitching, stabbing and burning character relieved temporarily by cold application and not by rest or motion.
- The patient shrieks on account of pain.
- Backache accompanied by great weakness.
Arnica:
- Generally, Chronic arthritis with a feeling of bruised soreness can indicate a need for this remedy.
- Pain is worse specifically from touch, and may occur in joints that were injured in the past.
Ruta graveolens:
- Arthritis with a feeling of great stiffness and lameness, worse from cold and damp, and worse from exertion often is relieved by this remedy.
- Tendons and the capsules of the joints may be affected.
- Besides this; Arthritis may have developed after overuse, from repeated wear and tear.
Kalmia latifolia:
- Intense arthritic pain that appears quite suddenly may indicate this medicine especially when the problems start in higher joints and extend to lower ones.
- Pain and inflammation often start in the shoulder, moving to the elbow, wrist and hand.
- The knees are also frequently affected.
- Discomfort is worse from motion and often worse at night.
Apis mellifica:
- This remedy can be helpful in acute conditions with redness, tenderness, also swelling.
- Joints feel hot and have stinging pain.
- The hands and knees are often affected.
- Warmth can aggravate the symptoms and cool applications bring relief.
Calcarea fluorica:
- This medicine is often indicated for arthritic pains that are improved especially by heat and motion.
- Joints become enlarged also hard, and nodosities or bone spurs may develop.
- Arthritis after chronic injury to joints often responds to Calcarea fluorica.
Calcarea carbonica:
- This remedy is often useful for arthritis in a person who is flabby or higher-weight person , and easily tired by exertion.
- Inflammation and soreness are worse from cold and dampness, and weakness or cramping in the extremities are often seen.
- Problems often focus on the knees when Calcarea is needed.
Sticta Pulmonaria:
- Rheumatism of right shoulder blade or joint, wrist joint, ankle joint and knee joint.
- It also reduces fluid in the joints. [6]
Diet & Regimen
Do’s and Dont’s
Tab Content
Terminology
Tab Content
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 25
- https://www.mayoclinic.org/diseases-conditions/osteoarthritis/symptoms-causes/syc-20351925
- https://www.healthline.com/health/osteoarthritis#osteoarthritis-symptoms
- https://www.webmd.com/osteoarthritis/guide/osteoarthritis-basics#1
- https://www.medicinenet.com/osteoarthritis/article.htm#how_do_health_care_professionals_diagnose_osteoarthritis
- http://homeopathyclinic.co.in/10-best-homeopathic-medicines-treatment-osteoarthritis/
FAQ
Frequently Asked Questions
What is Osteoarthritis?
Osteoarthritis (OA) is characterized by focal loss of articular cartilage, subchondral osteosclerosis, osteophyte formation at the joint margin, and remodeling of joint contour with enlargement of affected joints.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Osteoarthritis?
- Bryonia Alba
- Rhus Tox
- Kali Carb
- Arnica
- Ruta graveolens
- Kalmia latifolia
- Apis mellifica
- Calcarea fluorica
- Calcarea carbonica
- Sticta Pulmonaria
What causes Osteoarthritis?
- Heredity
- Obesity
- Injury
- Joint overuse
- Other diseases
What are the symptoms of Osteoarthritis?
- Pain: Insidious onset, intermittent, morning stiffness
- Restricted movement
- Palpable, sometimes audible, coarse crepitus
- Bony swelling around joint margins
- Deformity, usually without instability
- Either Joint-line or periarticular tenderness
- Muscle weakness also wasting
- Synovitis mild or absent
Give the types of Osteoarthritis?
- Generalised nodal OA
- Knee OA
- Hip OA
- Spine OA
- Early-onset OA
Also Search As
Frequently Asked Questions (FAQ)
XYZ
XXX
XYZ
XXX
XYZ
XXX
How can I find reputable homeopathy clinics or homeopathic doctors in my area?
You can found Homeopathic Clinic For XXXX by searching for
Specific city Examples are
You can also search for near you Examples are