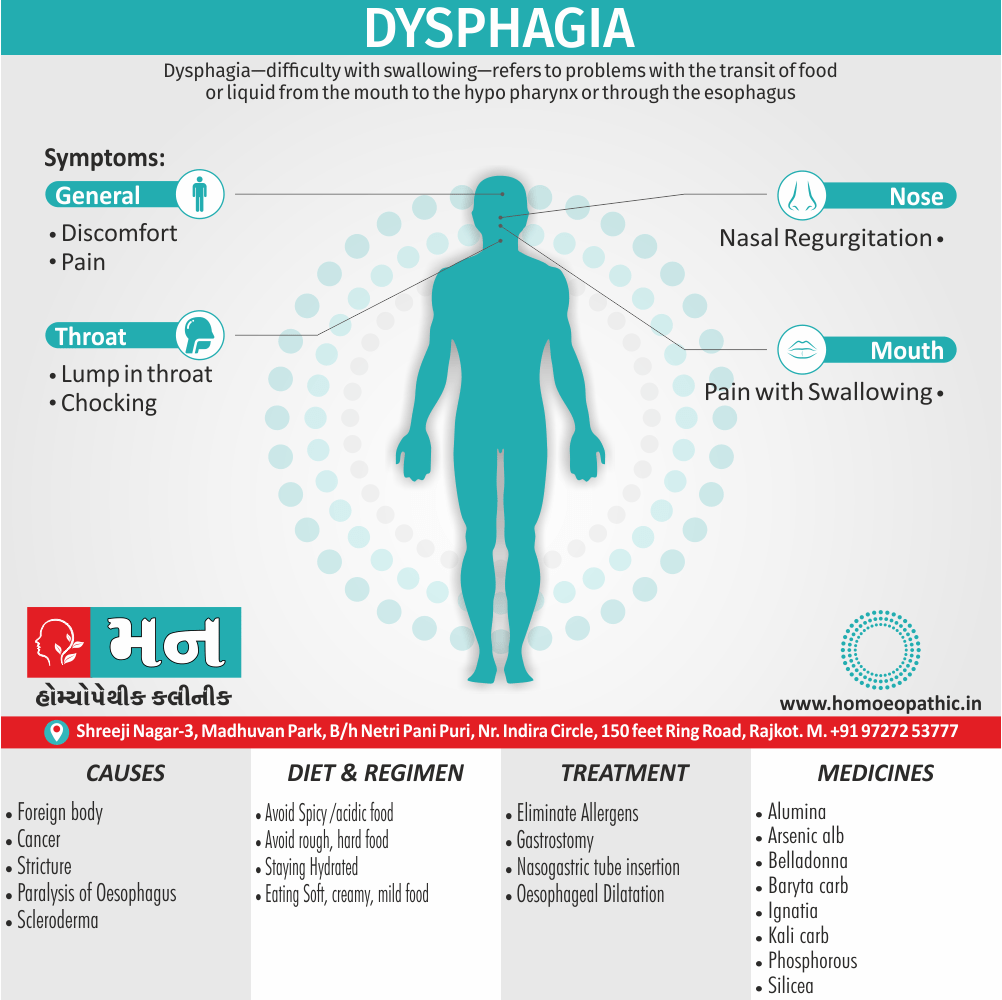
Overview of Dysphagia
Severe dysphagia can compromise nutrition, cause aspiration, also reduce quality of life. Additional terminology pertaining to swallowing dysfunction is as follows.
- Generally, Aphagia (inability to swallow) typically denotes complete esophageal obstruction, most commonly encountered in the acute setting of a food bolus or foreign body impaction.
- Moreover, Odynophagia refers to painful swallowing, typically resulting from mucosal ulceration within the oropharynx or esophagus. It commonly is accompanied by dysphagia, but the converse is not true.
- Globus pharyngeus is a foreign body sensation localized in the neck that does not interfere with swallowing and sometimes is relieved by swallowing.
- Besides this, Transfer dysphagia frequently results in nasal regurgitation and pulmonary aspiration during swallowing and is characteristic of oropharyngeal dysphagia.
- Phagophobia (in other words, fear of swallowing) and refusal to swallow may be psychogenic or related to anticipatory anxiety about food bolus obstruction, odynophagia, or aspiration.[3]
Causes of Dysphagia
In general, Swallowing is complex, involving many muscles and nerves. Any condition that weakens or damages the muscles also nerves used for swallowing or leads to a narrowing of the back of the throat or Esophagus can cause dysphagia.
Dysphagia generally falls into one of the following categories.
Esophageal dysphagia
Esophageal dysphagia refers to the sensation of food sticking or getting caught in the base of your throat or in your chest after you’ve started to swallow. Some of the causes of esophageal dysphagia include:
Achalasia
- When the lower esophageal muscle (i.e. sphincter) doesn’t relax properly to let food enter the stomach, it can cause food to come back up into the throat.
- Furthermore, Muscles in the wall of the esophagus might be weak as well, a condition that tends to worsen over time.
Diffuse spasm
- This condition causes high-pressure, poorly coordinated contractions of the esophagus, usually after swallowing.
- In detail, Diffuse spasm affects the involuntary muscles in the walls of the lower esophagus.
Esophageal stricture
- A narrowed esophagus (stricture) can trap large pieces of food.
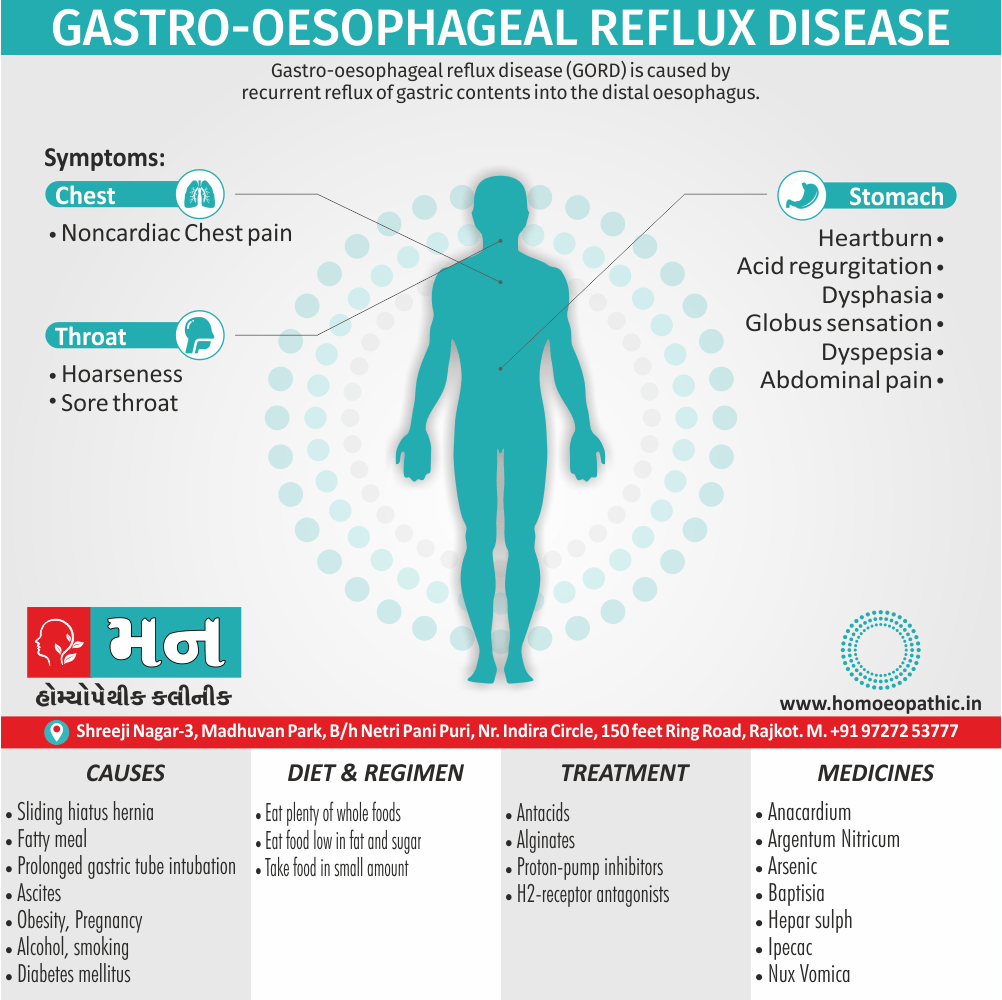
- Tumors or scar tissue, often caused by gastroesophageal reflux disease (in other words, GERD), can cause narrowing.
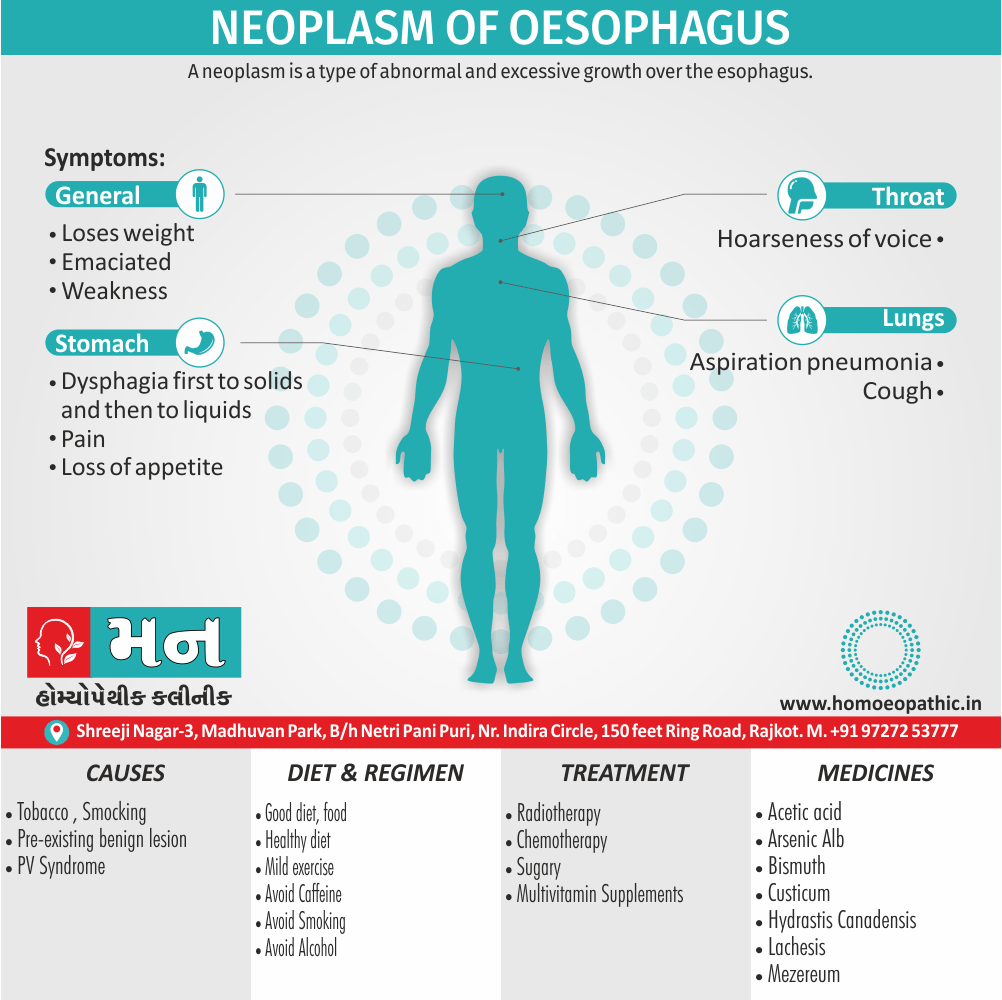
Esophageal tumors
- In brief, Difficulty swallowing tends to get progressively worse especially, when esophageal tumors are present due to narrowing of the esophagus.
Foreign bodies
- Generally, Sometimes food or another object can partially block the throat or esophagus.
- Additionally, Older adults with dentures and people who have difficulty chewing their food may be more likely to have a piece of food become lodged in the throat or esophagus.
Esophageal ring
- In brief, A thin area of narrowing in the lower esophagus can cause difficulty swallowing solid foods off and on.
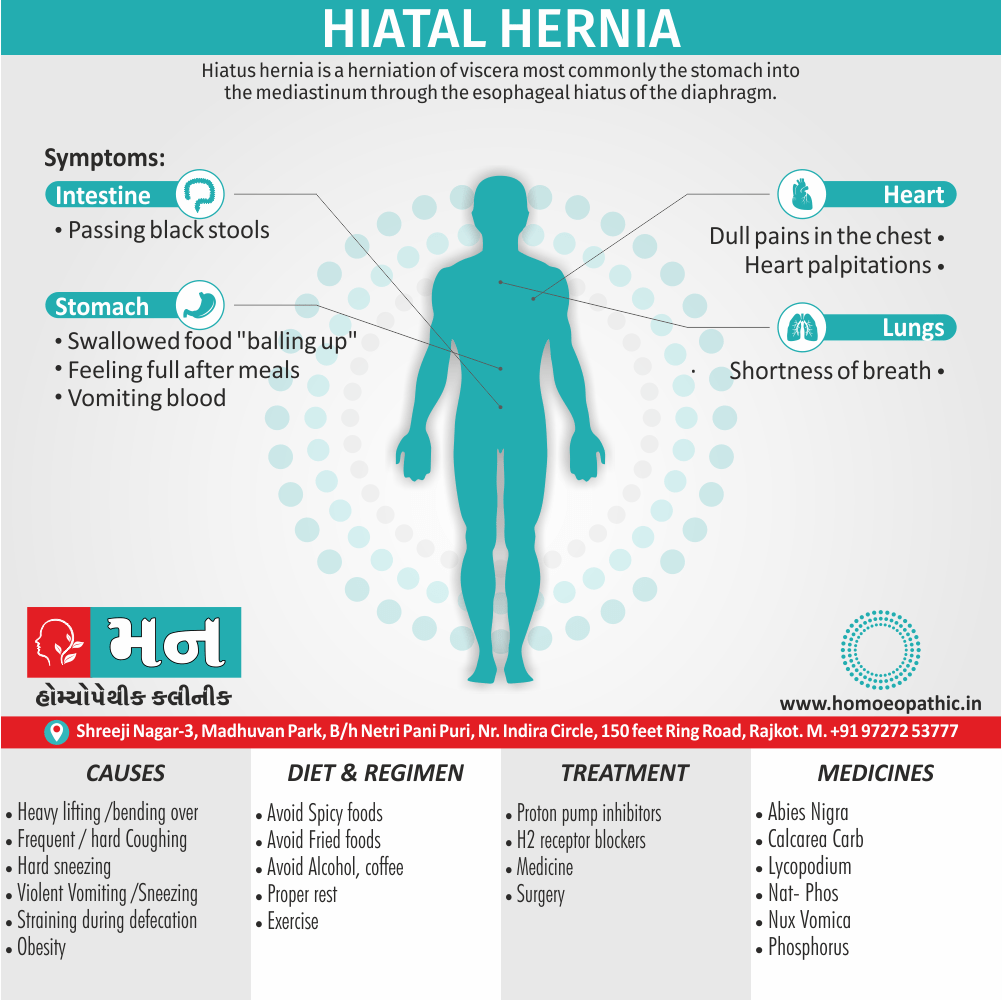
GERD
- Damage to esophageal tissues from stomach acid backing up into the esophagus can lead to either, spasm or scarring and narrowing of the lower esophagus.
Eosinophilic esophagitis
- This condition, which might be related to a food allergy, is caused by too many cells called eosinophils in the esophagus.
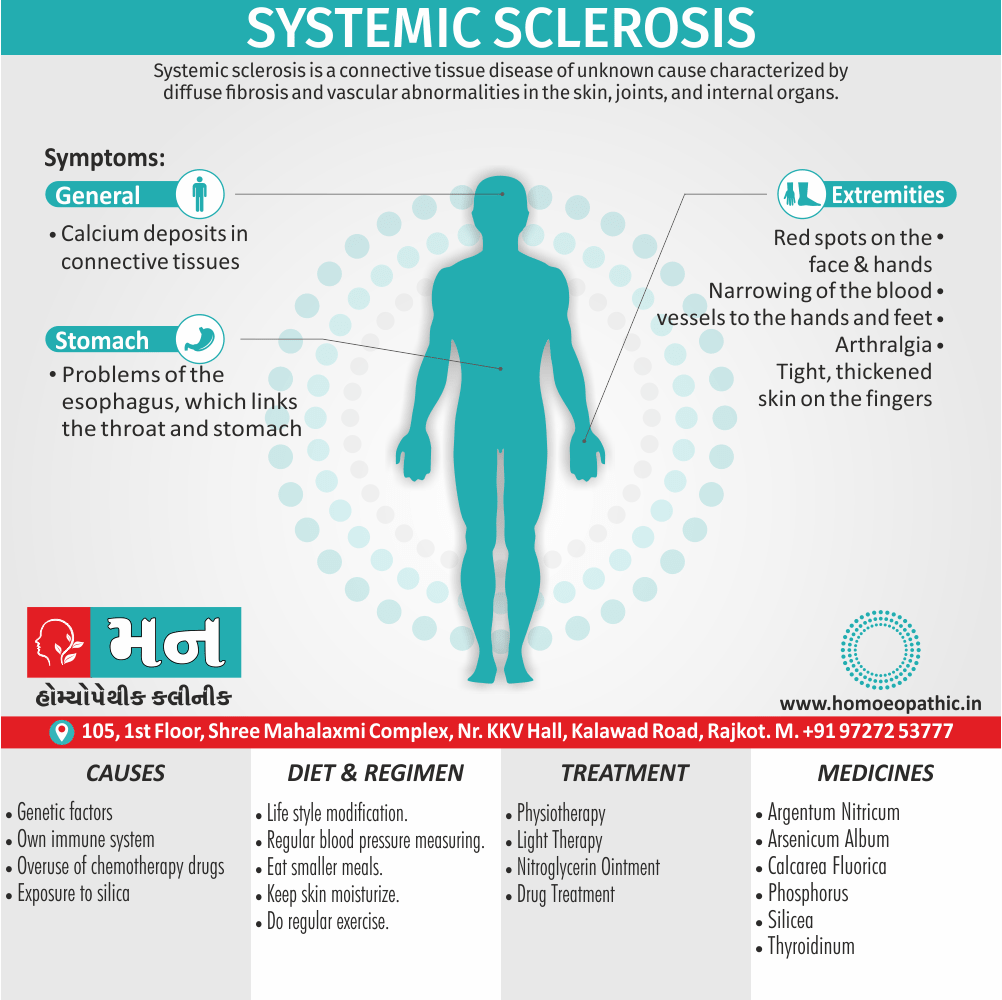
Scleroderma
- Development of scar-like tissue, causing stiffening also hardening of tissues, can weaken the lower esophageal sphincter.
- As a result, acid backs up into the esophagus and causes frequent heartburn.
Radiation therapy
- All in all, This cancer treatment can lead to inflammation also scarring of the esophagus.
Oropharyngeal dysphagia
Generally, Certain conditions can weaken the throat muscles, making it difficult to move food from your mouth into your throat and Esophagus when you start to swallow.
You might choke, gag or cough when you try to swallow or have the sensation of food or fluids going down your windpipe (in other words, trachea) or up your nose. Additionally, This can lead to pneumonia.
Causes of oropharyngeal dysphagia i.e.:
Neurological disorders
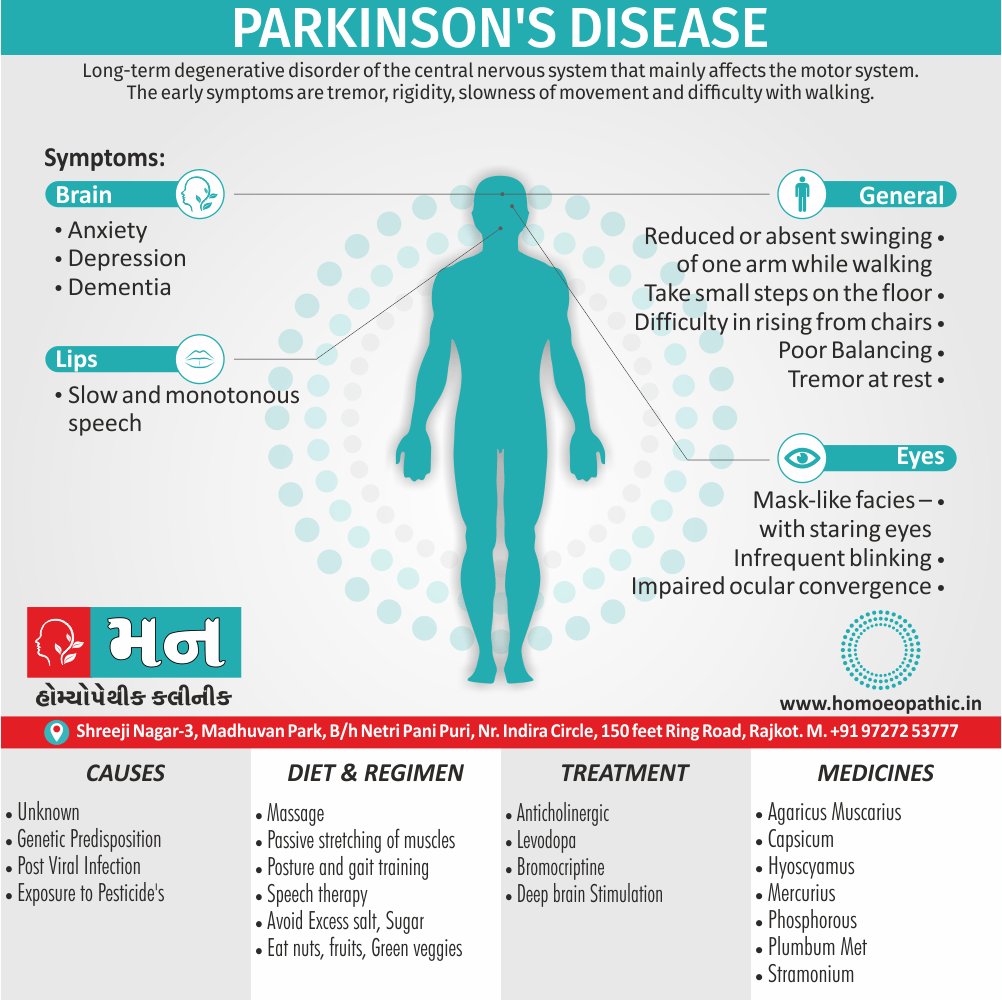
- Certain disorders — e.g. multiple sclerosis, muscular dystrophy and Parkinson’s disease — can cause dysphagia.
Neurological damage
- Sudden neurological damage, e.g. from a stroke or brain or spinal cord injury, can affect the ability to swallow.
Pharyngoesophageal diverticulum (in other words, Zenker’s diverticulum)
- A small pouch that forms and collects food particles in the throat, often just above the esophagus, leads to difficulty swallowing, gurgling sounds, bad breath, also repeated throat clearing or coughing.
Cancer
- Certain cancers and some cancer treatments, e.g. radiation, can cause difficulty swallowing.[3][4]
Risk factors of Dysphagia
The following are risk factors for dysphagia:
Aging
- Due to natural aging and normal wear and tear on the esophagus as well as a greater risk of certain conditions, such as stroke or Parkinson’s disease, older adults are at higher risk of swallowing difficulties. But dysphagia isn’t considered a normal sign of aging.
Certain health conditions
- People with certain neurological or nervous system disorders are more likely to have difficulty swallowing.[4]
Types of Dysphagia
There are two types of dysphagia:
Oropharyngeal dysphagia (“high” dysphagia)
- It occurs when a person has difficulty moving food to the back of the mouth and starting the swallowing process.
- This is typically caused by a neurological problem that has weakened the nerves and muscles.
Esophageal dysphagia (“low” dysphagia)
- It occurs when food or liquid stops in the esophagus, usually because of a blockage or irritation.[4]
Sign & Symptoms of Dysphagia
- Pain while swallowing
- Inability to swallow
- A sensation of food getting stuck in the throat or chest or behind the breastbone (sternum)
- Drooling
- Hoarseness
- Food coming back up (regurgitation)
- Frequent heartburn
- Food or stomach acid backing up into the throat
- Weight loss
- Coughing or gagging when swallowing
- Pain while Swallowing Solid or Liquid
- Regurgitation of food [4]
Clinical examination of Dysphagia
Appearance of the Patient
- Patients with dysphagia usually appear in discomfort.
Vital Signs
- Normal
Skin
- Skin examination of patients with dysphagia is usually normal.
HEENT
- HEENT examination of patients with dysphagia is usually normal.
Neck
- Neck examination of patients with dysphagia is usually normal, but may presents with masses or swelling of the neck depending on the underlying cause.
- Laryngeal Cancer
- Thyroid goiters
- Esophageal cancers
Lungs
- Pulmonary examination of patients with dysphagia is usually normal.
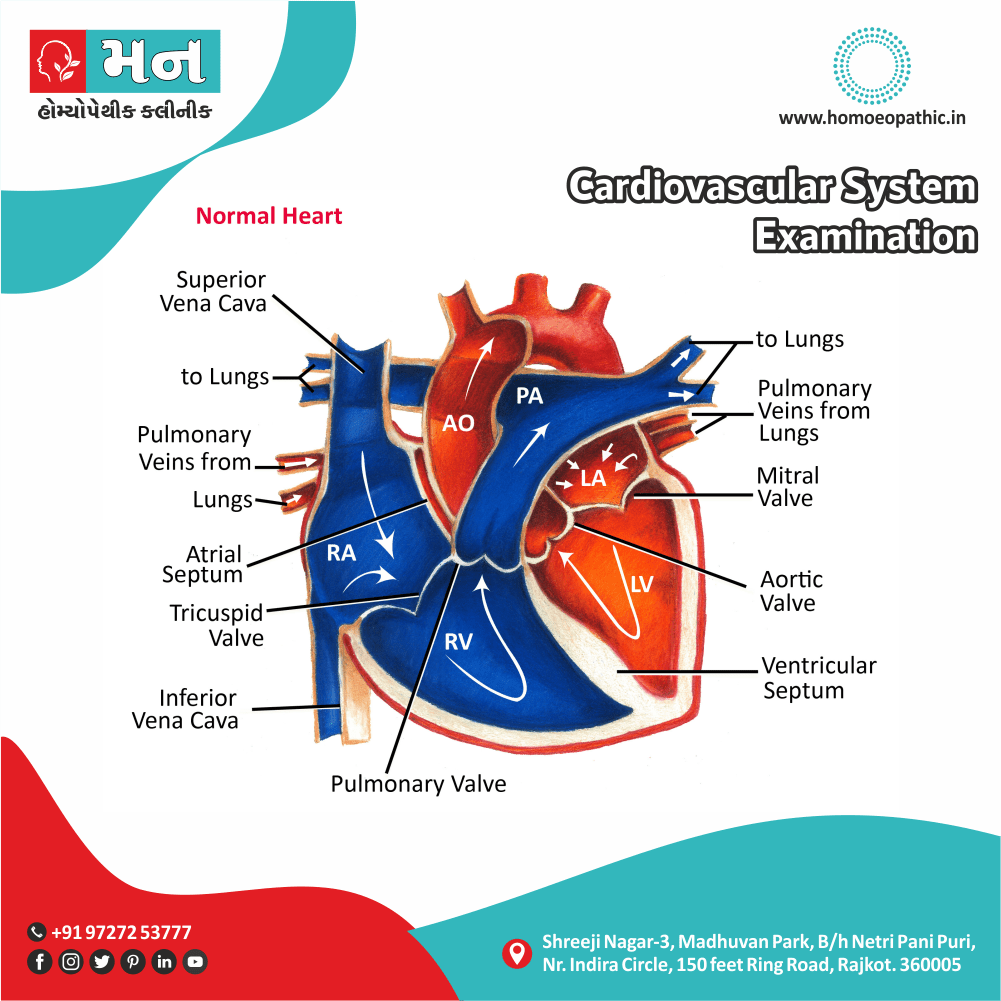
Heart
- Cardiovascular examination of patients with dysphagia is usually normal.
Abdomen
- Abdominal examination of patients with dysphagia is usually normal.
Back
- Back examination of patients with dysphagia is usually normal.
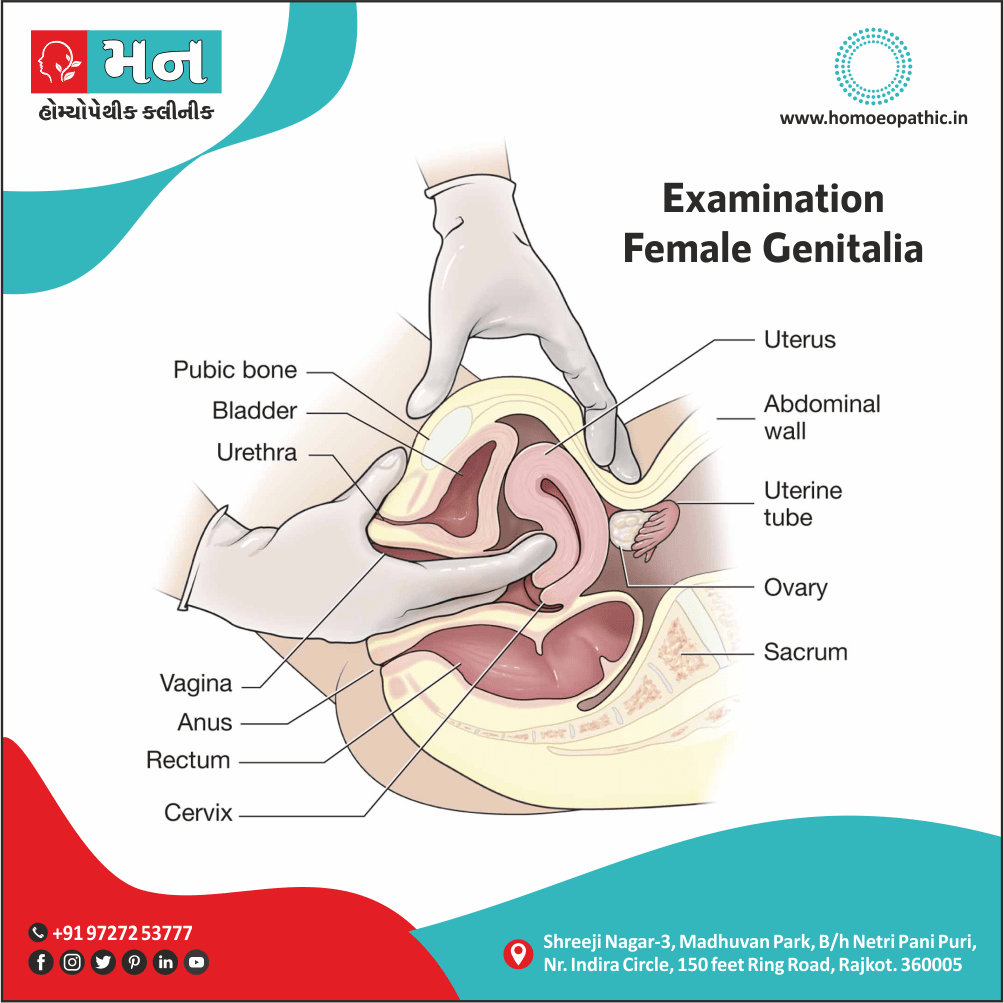
Genitourinary
- Genitourinary examination of patients with dysphagia is usually normal.
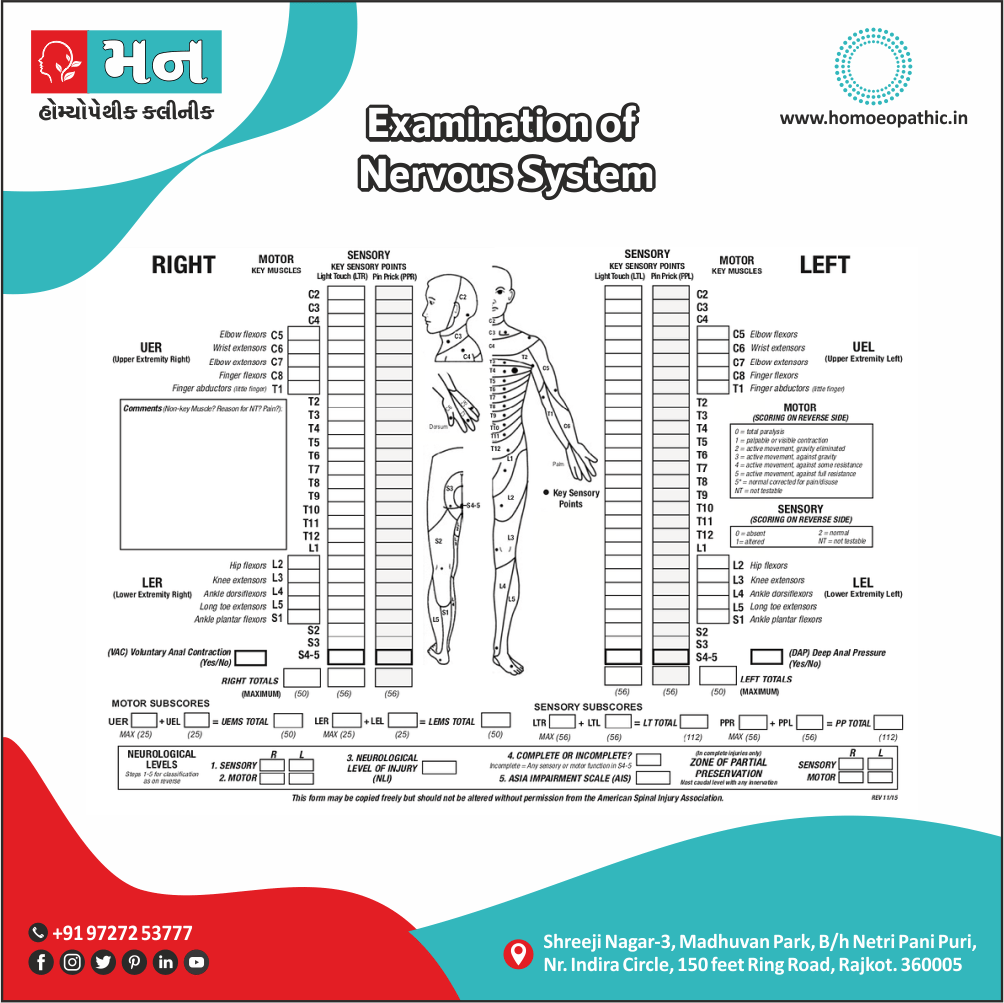
Neuromuscular
- Neuromuscular examination of patients with dysphagia is usually dependent on the underlying disease.
- Stroke
- Neuromuscular disorders
Extremities
- Extremities examination of patients with dysphagia is usually normal. (5)
Investigation of Dysphagia
There are no diagnostic laboratory findings associated with dysphagia per se. However, in certain diseases leading to dysphagia, laboratory evaluation is done to look for the underlying disease.
Such diseases include the following:
- Myasthenia gravis
- Thyrotoxicosis
- Inflammatory myopathies
- Toxic myopathies
Following laboratory tests are done for the diagnosis of these diseases:
- Acetylcholine receptor (AChR) antibodies
- Thyroid function tests
- Muscle enzyme essays (5)
Diagnosis of Dysphagia
Your health care provider will likely ask you for a description and history of your swallowing difficulties, perform a physical examination, and use various tests to find the cause of your swallowing problem.
Tests can include:
X-ray with a contrast material (barium X-ray)
- You drink a barium solution that coats your Esophagus, making it easier to see on X-rays.
- Your health care provider can then see changes in the shape of your Esophagus and can assess the muscular activity.
- Your health care provider might also have you swallow solid food or a pill coated with barium to watch the muscles in your throat as you swallow or to look for blockages in your Esophagus that the liquid barium solution might not identify.
Dynamic swallowing study
- You swallow barium-coated foods of different consistencies. This test provides an image of these foods as they travel down your throat.
- The images might show problems in the coordination of your mouth and throat muscles when you swallow and determine whether food is going into your breathing tube.
A visual examination of your Esophagus (endoscopy)
- A thin, flexible lighted instrument (endoscope) is passed down your throat so that your health care provider can see your Esophagus.
- Your health care provider might take biopsies of the Esophagus to look for inflammation, eosinophilic esophagitis, narrowing or a tumor.
Fiber-optic endoscopic evaluation of swallowing (FEES)
- Your health care provider might examine your throat with a special camera and lighted tube (endoscope) as you try to swallow.
Esophageal muscle test (manometry)
- In manometry a small tube is inserted into your Esophagus and connected to a pressure recorder to measure the muscle contractions of your Esophagus as you swallow.
Imaging scans
- These can include a CT scan, which combines a series of X-ray views and computer processing to create cross-sectional images of your body’s bones and soft tissues, or an MRI scan, which uses a magnetic field and radio waves to create detailed images of organs and tissues.
Physical examination
- Physical examination is important in the evaluation of oral and pharyngeal dysphagia because dysphagia is usually only one of many manifestations of a more global disease process.
- Signs of bulbar or pseudobulbar palsy, including dysarthria, dysphonia, ptosis, tongue atrophy, and hyperactive jaw jerk, in addition to evidence of generalized neuromuscular disease, should be elicited.
- The neck should be examined for thyromegaly.
- A careful inspection of the mouth and pharynx should disclose lesions that may interfere with passage of food.
- Missing dentition can interfere with mastication and exacerbate an existing cause of dysphagia.
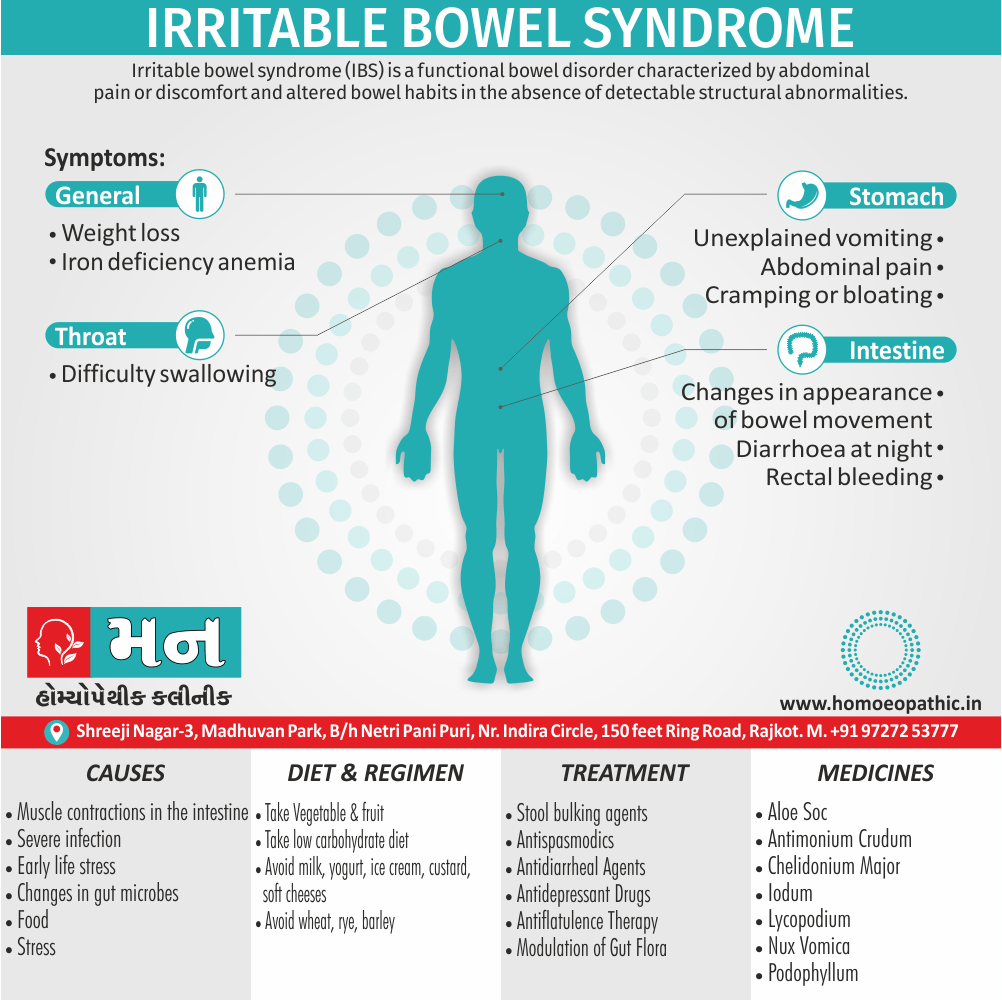
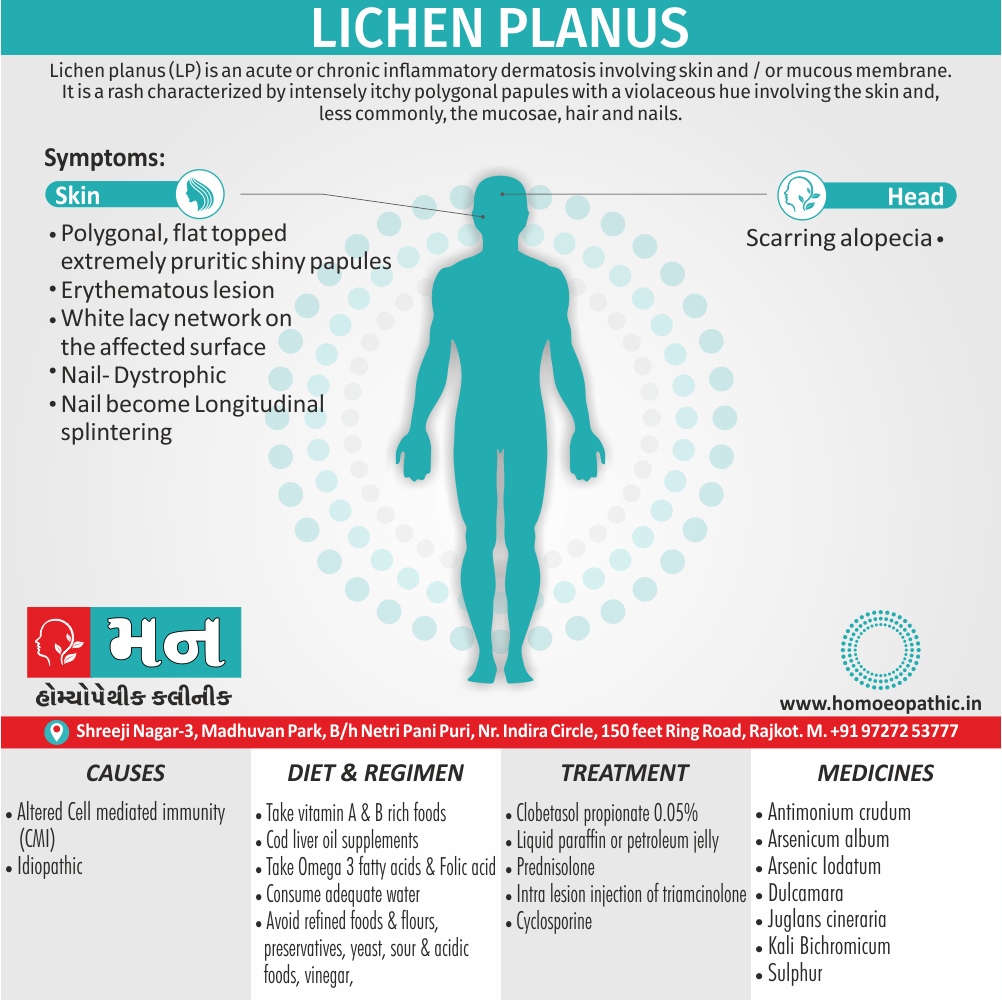
- Physical examination is less helpful in the evaluation of esophageal dysphagia as most relevant pathology is restricted to the esophagus. The notable exception is skin disease. Changes in the skin may suggest a diagnosis of scleroderma or mucocutaneous diseases such as pemphigoid, lichen planus and epidermolysis bullosa, all of which can involve the esophagus. [3][4]
Differntial diagnosis of Dysphagia
- Plummer-Vinson syndrome
- Esophageal stricture
- Zenker’s diverticulum
- Esophageal carcinoma
- Stroke
- GERD
- Esophageal web
- Diffuse esophageal spasm
- Achalasia
- Systemic sclerosis (5)
Treatment
Treatment for dysphagia depends on the type or cause of your swallowing disorder.
Oropharyngeal dysphagia
For oropharyngeal dysphagia, your health care provider might refer you to a speech or swallowing therapist. Therapy might include:
Learning exercises
- Certain exercises might help coordinate your swallowing muscles or restimulate the nerves that trigger the swallowing reflex.
Learning swallowing techniques
- You might also learn ways to place food in your mouth or position your body and head to help you swallow.
- Exercises and new swallowing techniques might help if your dysphagia is caused by neurological problems such as Alzheimer’s disease or Parkinson’s disease.
Esophageal dysphagia
Treatment approaches for esophageal dysphagia might include:
Esophageal dilation
- For a tight esophageal sphincter (in other words; achalasia) or an esophageal stricture, your health care provider might use an endoscope with a special balloon attached to gently stretch and expand your esophagus or pass a flexible tube or tubes to stretch the esophagus (dilation).
Surgery
- For an esophageal tumor, achalasia or pharyngoesophageal diverticulum, you might need surgery to clear your esophageal path.
Medications
- Difficulty swallowing associated with GERD can be treated with prescription oral medications to reduce stomach acid.
- You might need to take these medications for a long time.
- Corticosteroids might be recommended for eosinophilic esophagitis. For esophageal spasm, smooth muscle relaxants might help.
Diet
- Your health care provider might prescribe a special diet to help with your symptoms, depending on the cause of the dysphagia.
- If you have eosinophilic esophagitis, diet might be used as treatment.
Severe dysphagia
- If difficulty swallowing prevents you from eating also drinking enough also treatment doesn’t allow you to swallow safely, your health care provider might recommend a feeding tube.
- A feeding tube provides nutrients without the need to swallow.
Surgery
- Surgery might be needed to relieve swallowing problems caused by throat narrowing or blockages, including bony outgrowths, vocal cord paralysis, pharyngoesophageal diverticula, GERD and achalasia, or to treat esophageal cancer.
- Speech and swallowing therapy is usually helpful after surgery.
The type of surgical treatment depends on the cause of dysphagia. Some examples are:
- Laparoscopic Heller myotomy
- Peroral endoscopic myotomy (in other words, POEM)
- Esophageal dilation
- Stent placement
- Onabotulinumtoxin [3][4]
Prevention of Dysphagia
General preventive measures for dysphagia include:
- Following a healthy diet
- Alcohol and smoking cessation
- Regular exersice
- Revising medications
- Travel precautions (5)
Complications of Dysphagia
Difficulty swallowing can lead to:
- Malnutrition, weight loss and dehydration
- Aspiration pneumonia
- Choking- Food stuck in the throat can cause choking [4]
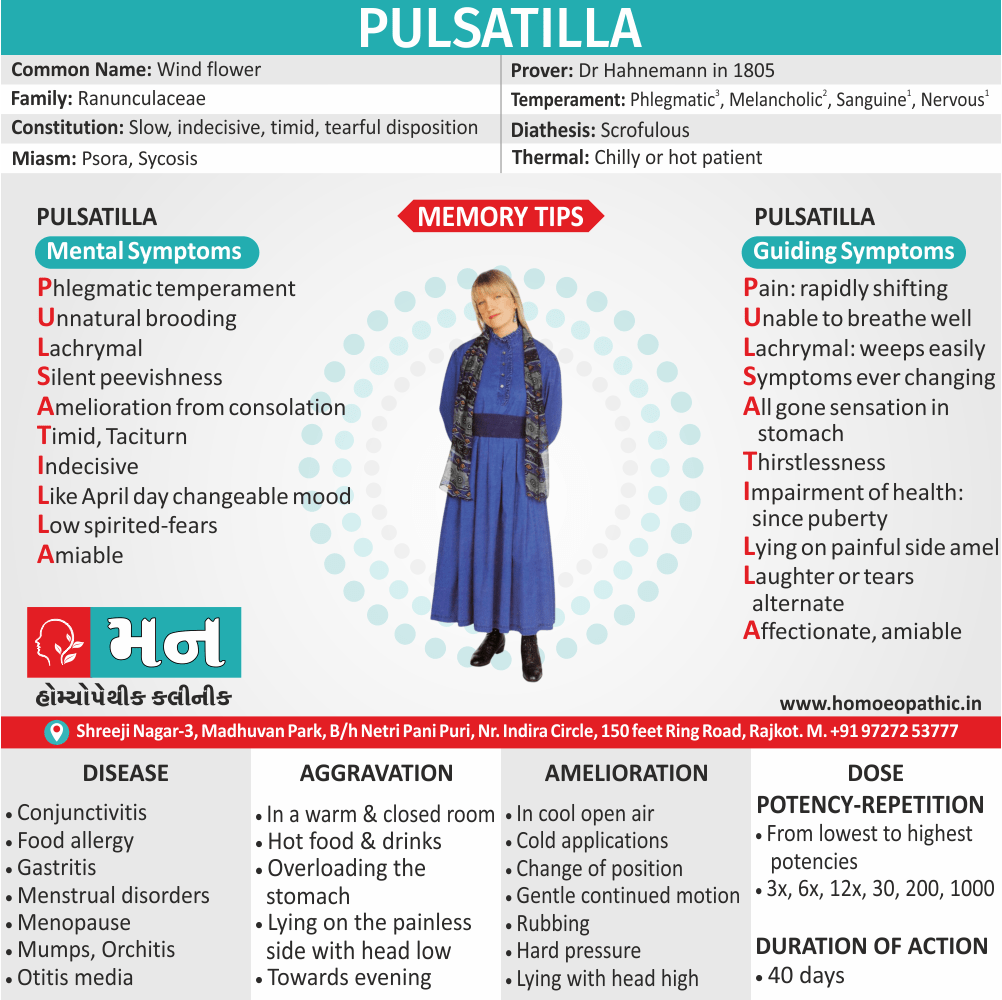
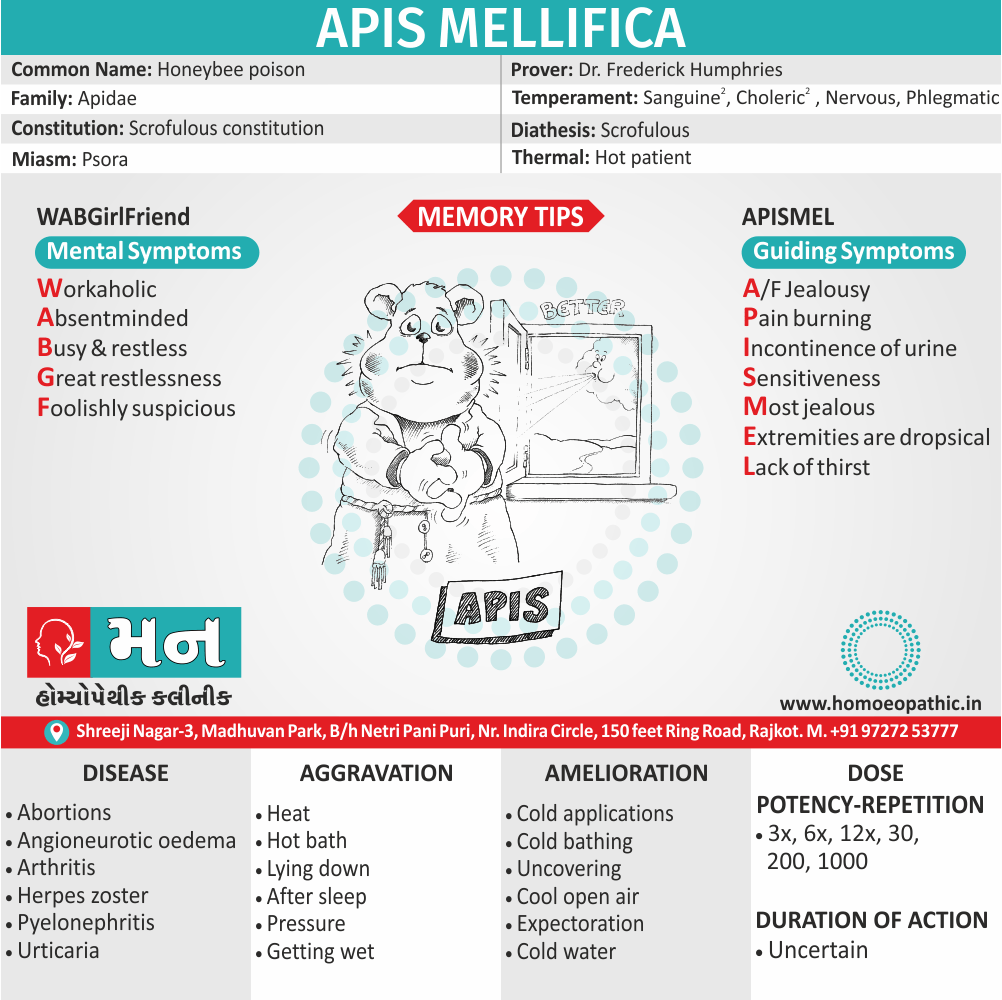
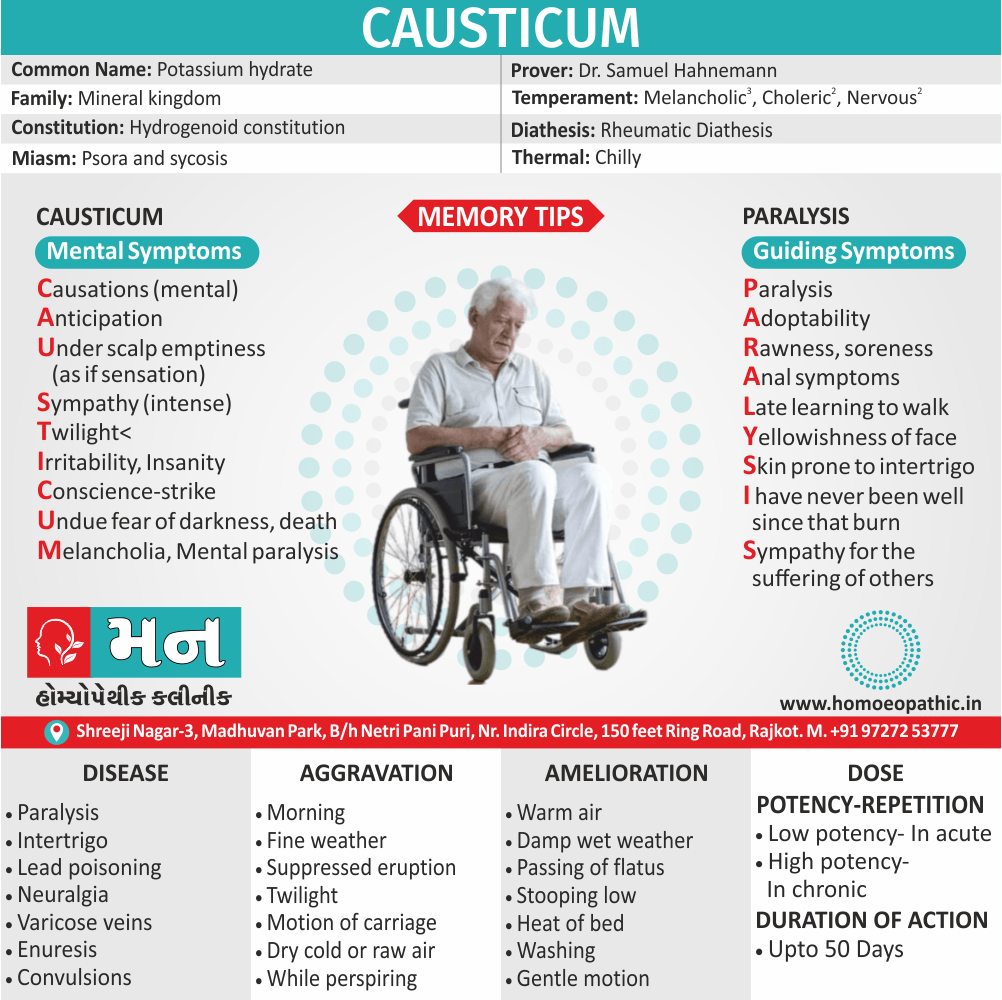
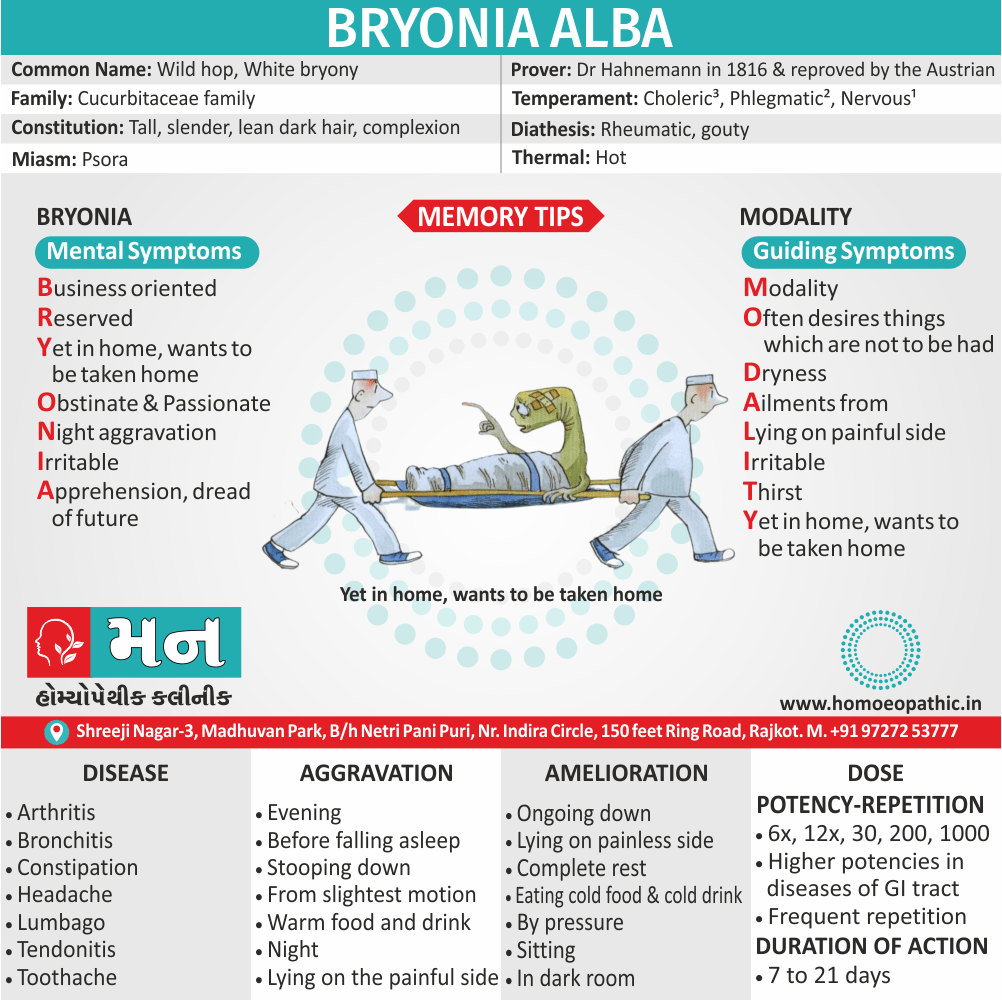
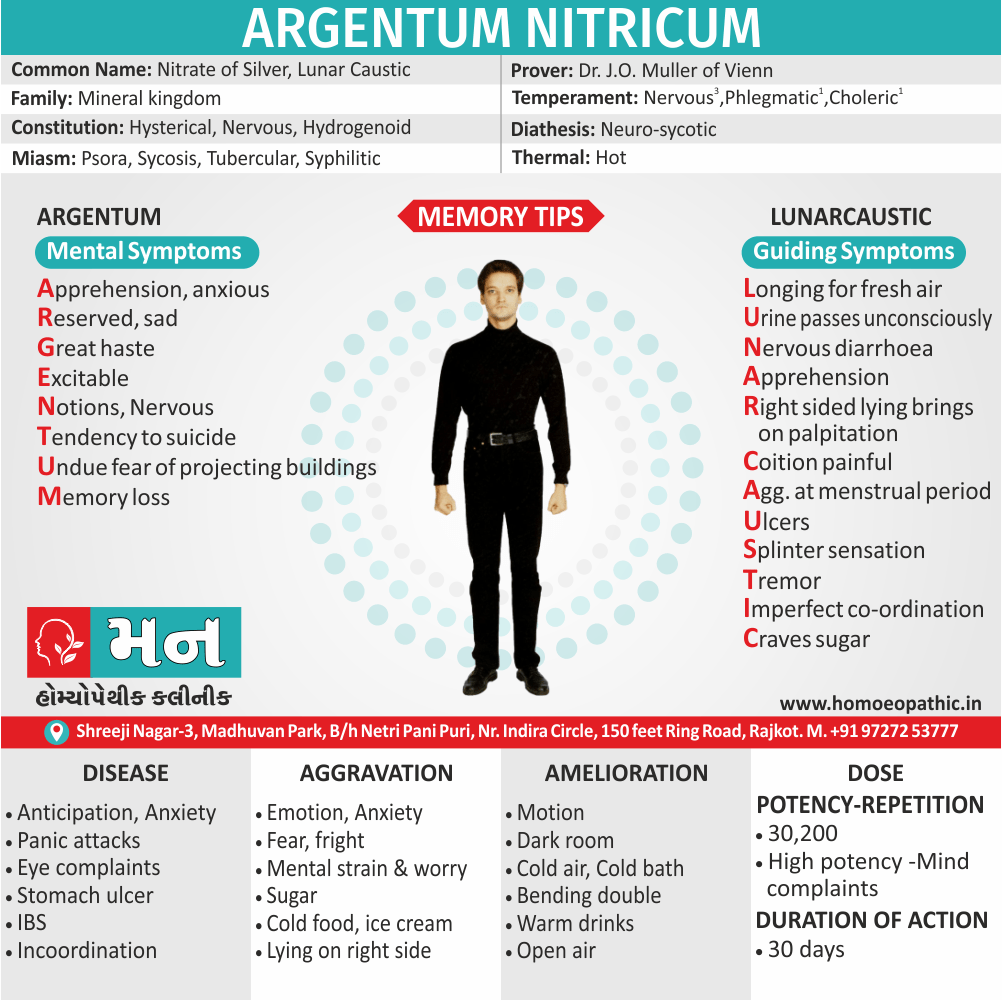
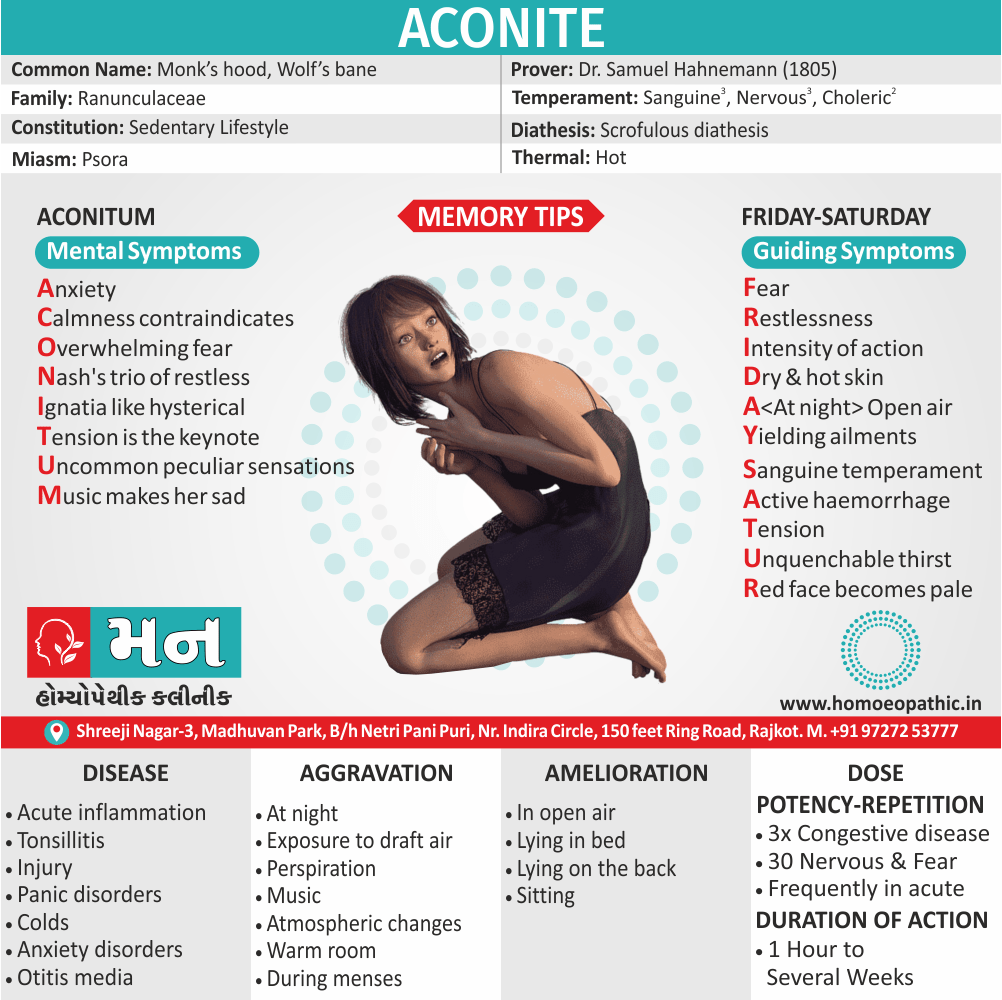
Homeopathic Treatment of Dysphagia
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
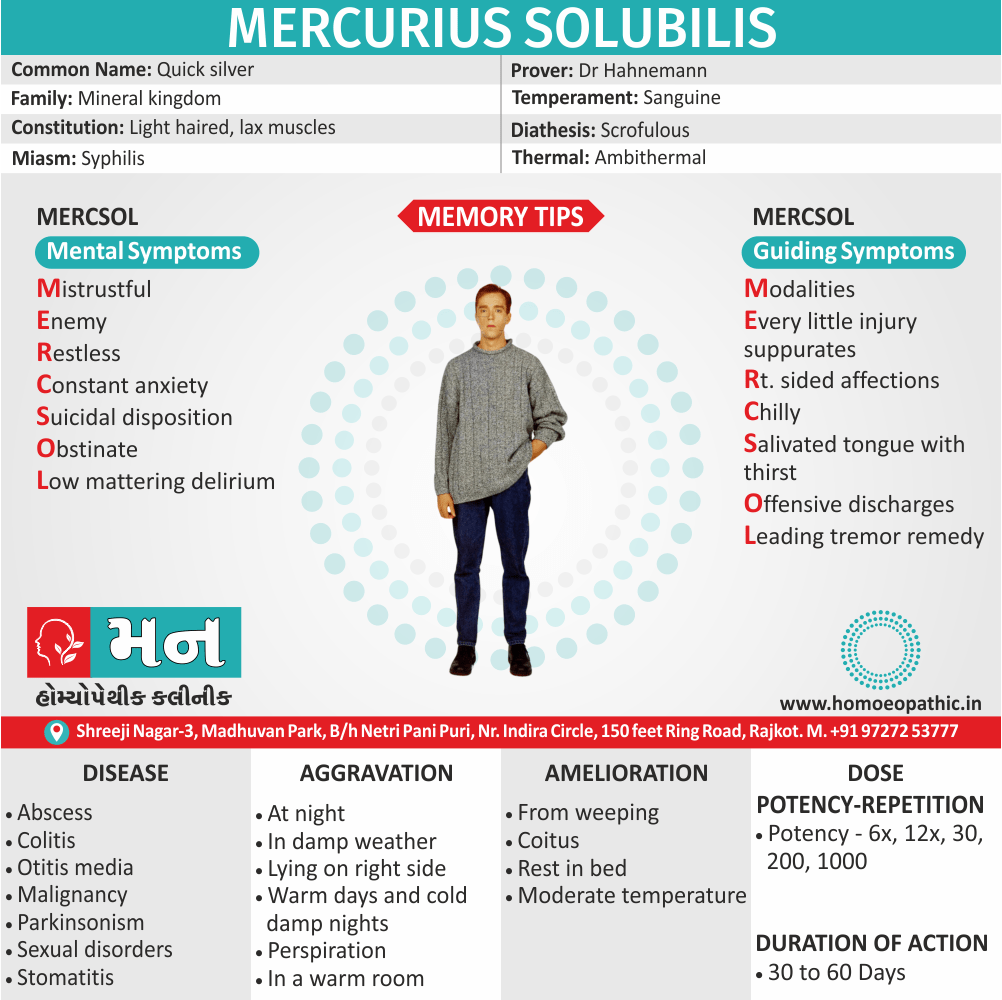
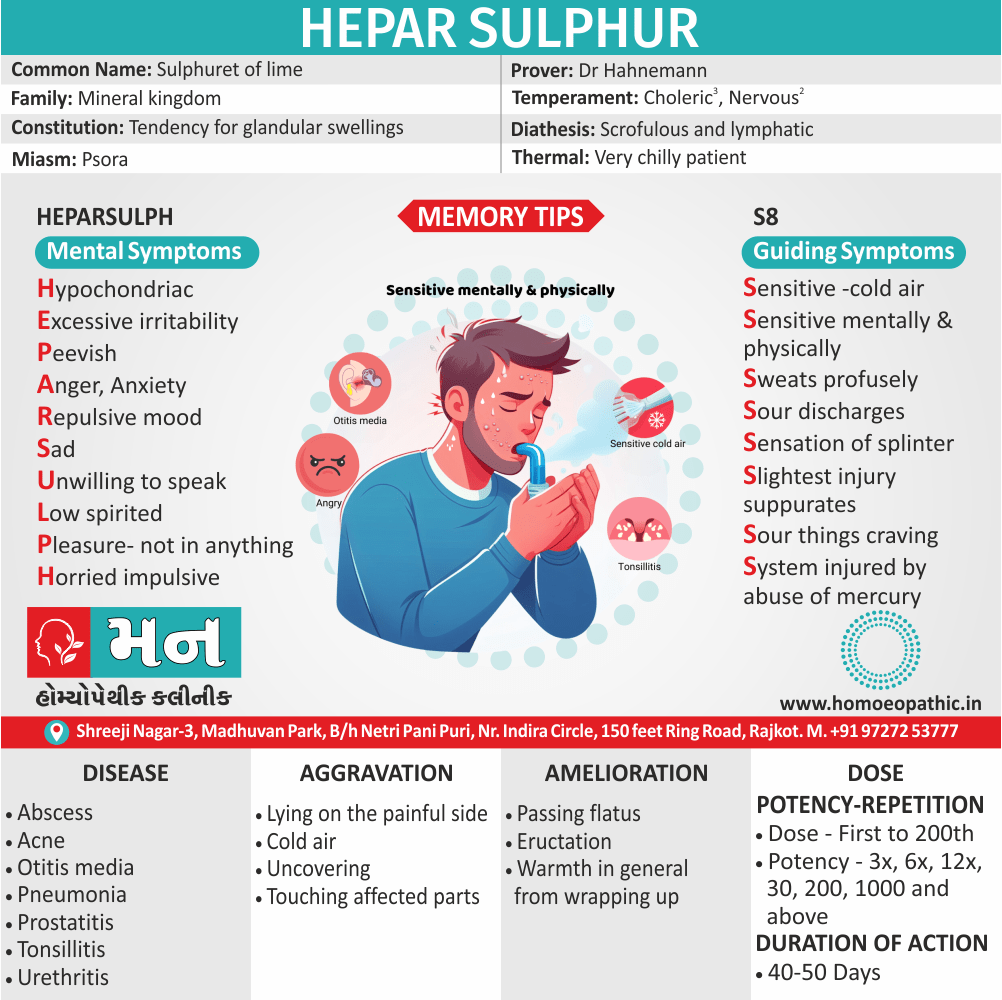
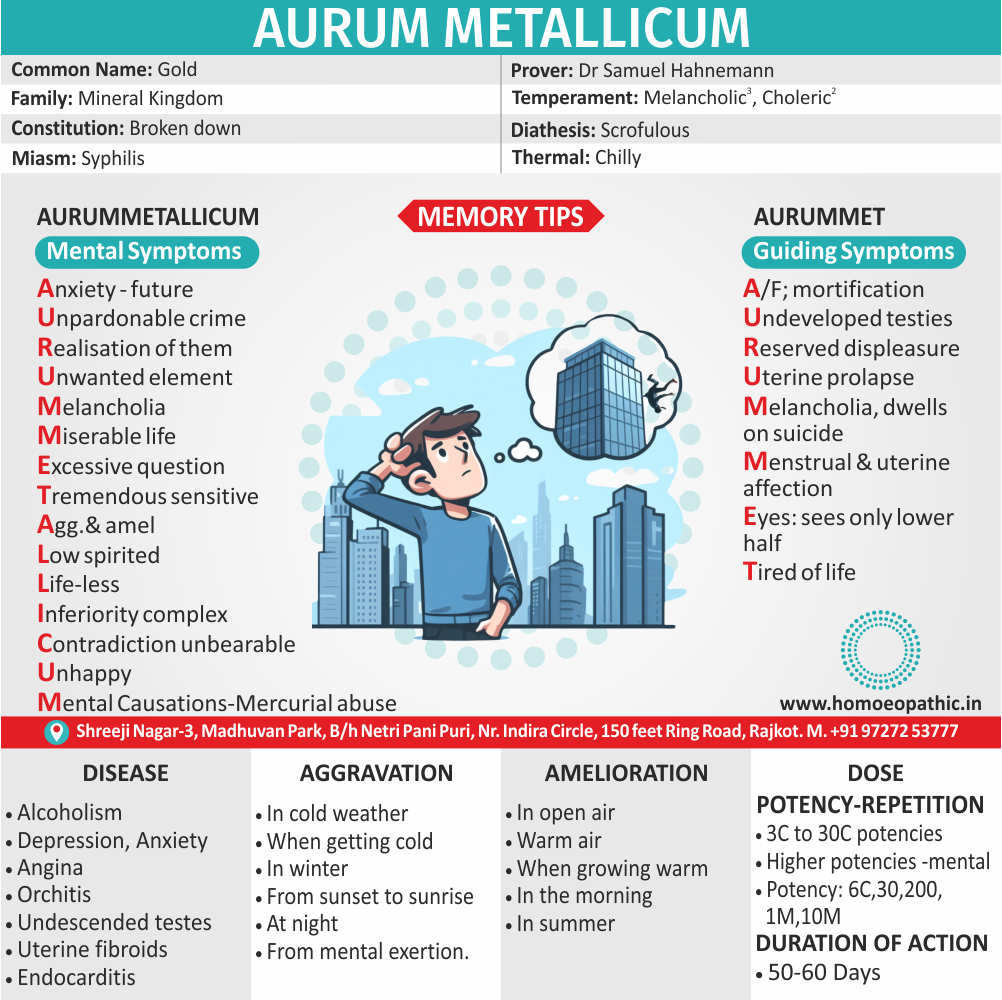
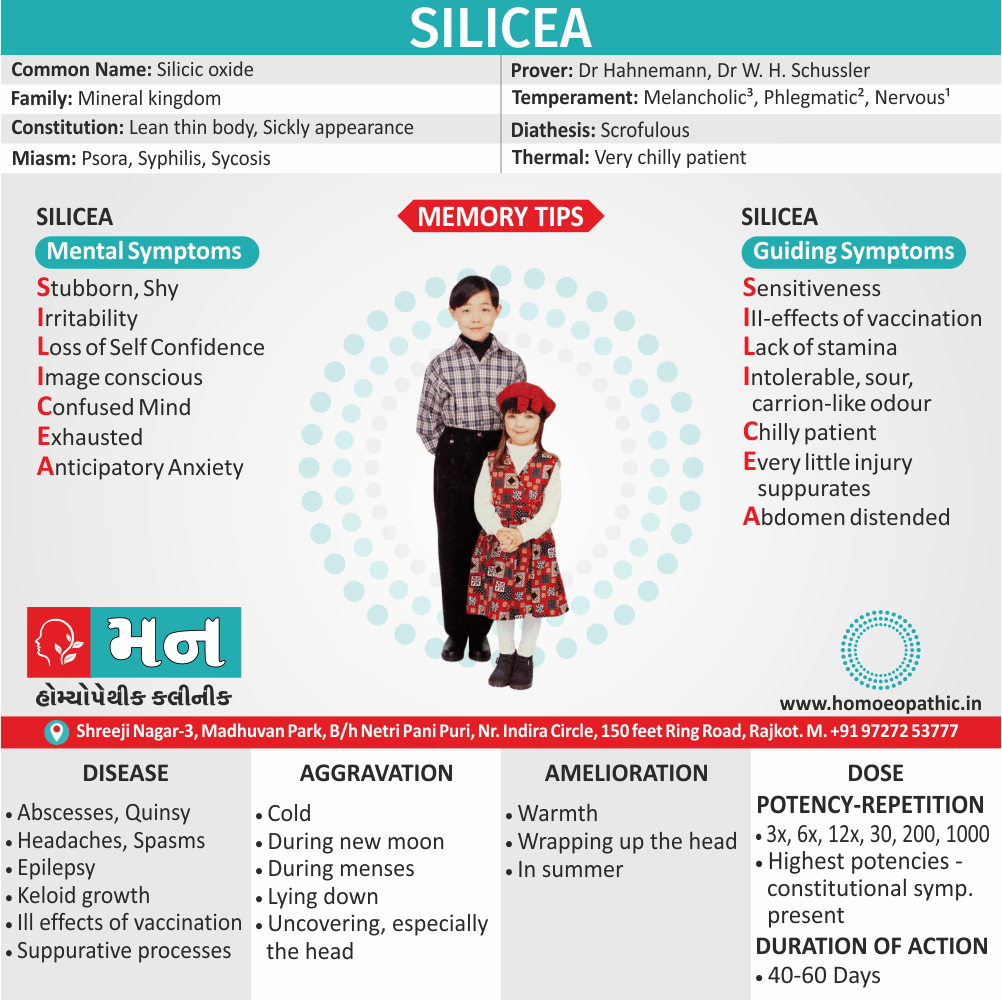
Homeopathic Medicines for Dysphagia:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicine:
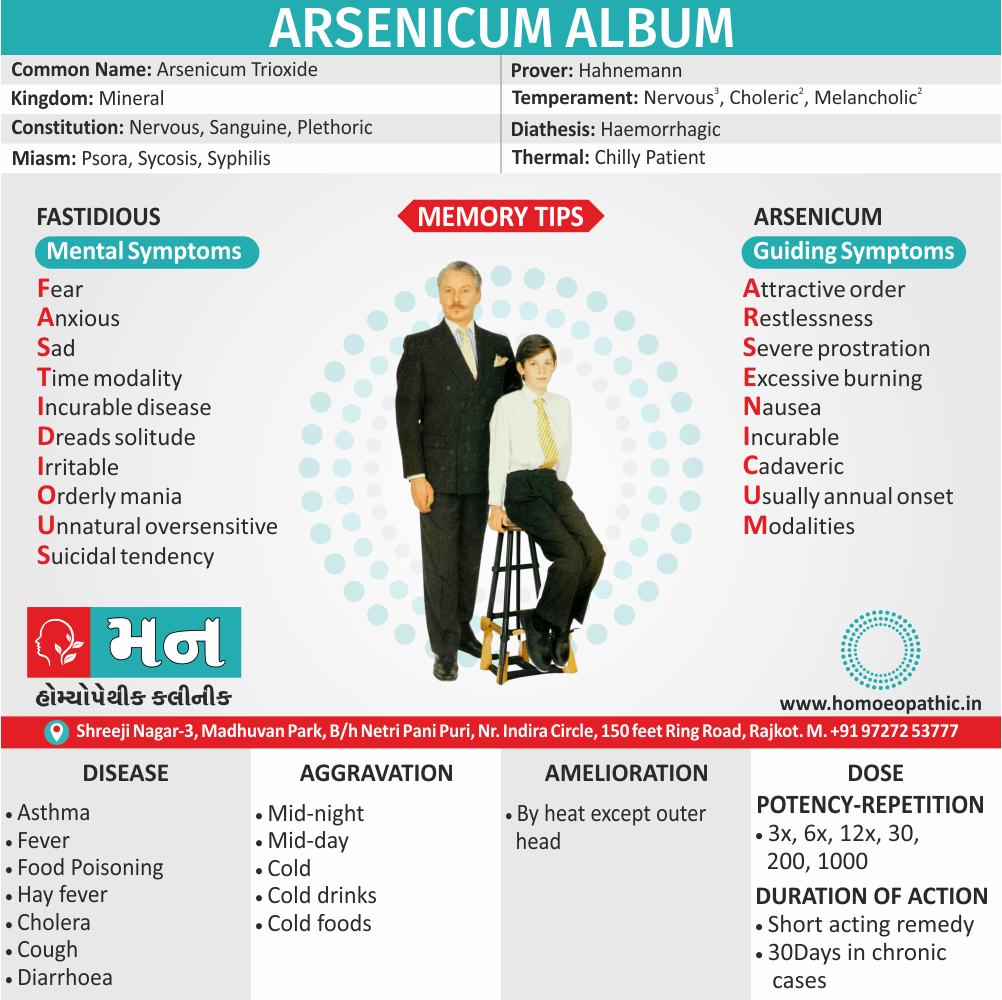
Arsenicum Album
- Throat swollen, constricted, burning, also unable to swallow.
- In detail, Everything swallowed seems to lodge in the esophagus, which seems closed.
- Worse – cold, wet weather, cold food and drinks. Better – warm drinks, heat.[1]
Alumina
- Dry, sore throat. Additionally, Food cannot pass esophagus contracted.
- As if either splinter or plug in throat.
- Worse – periodically, in morning. whereas Better -on awakening.
Baptisia
- In general, Constriction, contraction of Esophagus.
- Great difficulty in swallowing solid food.
- Can swallow liquids only.
- Contraction at cardiac orifice.
- Painless sore throat also offensive discharge.
- Worse – humid heat, fog.
Baryta carb
- Can only swallow liquids.
- Spasm of esophagus as soon as food enters esophagus, causes gagging also choking.
- Feeling of a plug-in pharynx.
- Smarting pain when swallowing. Worse – empty swallowing. [1]
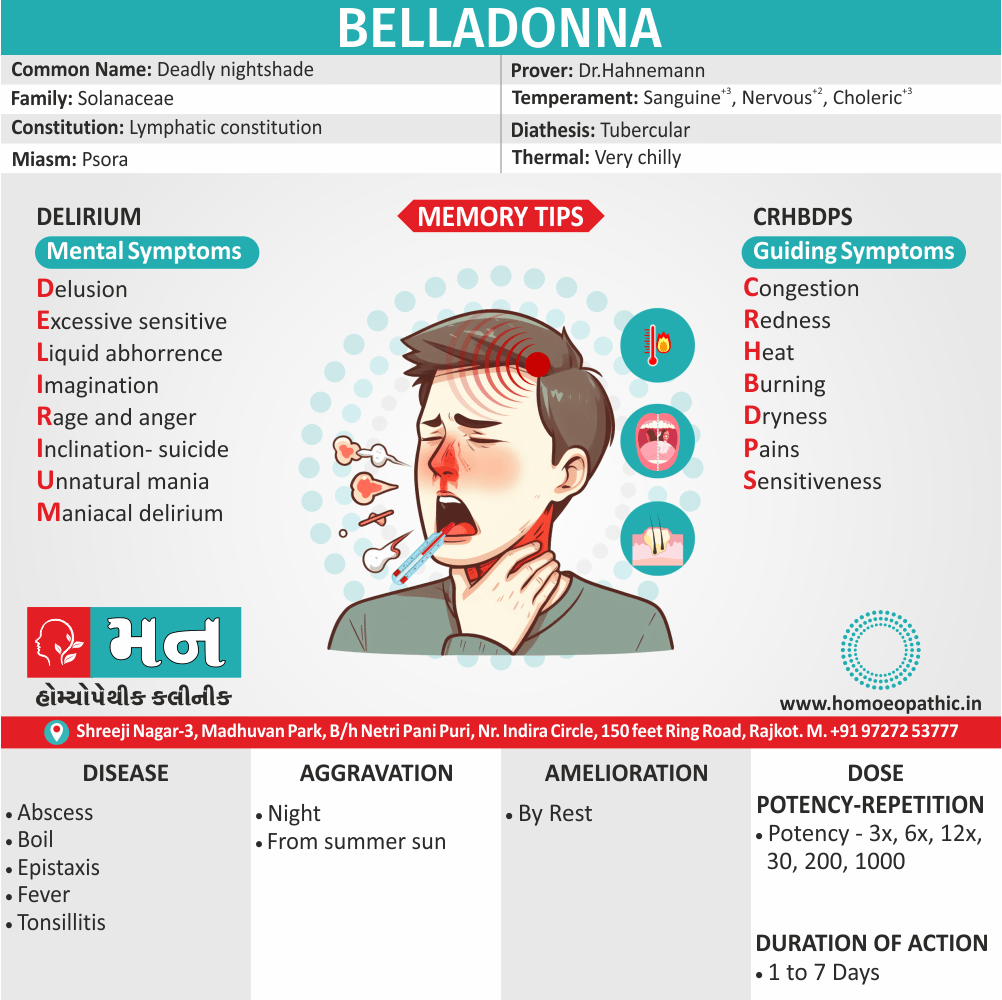
Belladonna
- Difficult deglutition, worse liquids, sensation of a lump, esophagus dry.
- Feels contracted, Spasms in throat, Continual inclination to swallow, Scraping sensation.
- Muscles of deglutition, very sensitive, great pain swallowing, inability to swallow.
- Worse -liquid, on the other hand, Better – semi erect.
- Besides this, Belladonna works well when a person having dysphagia has to drink water to help swallow food.
- There is also a tendency to choke easily while swallowing. Lastly, The food may go down the wrong way.
Cicuta
- Throat feels as if grown together.
- Spasms of esophagus cannot swallow.
- Effects on esophagus from swallowing sharp pieces of bone.
- Worse – from touch.
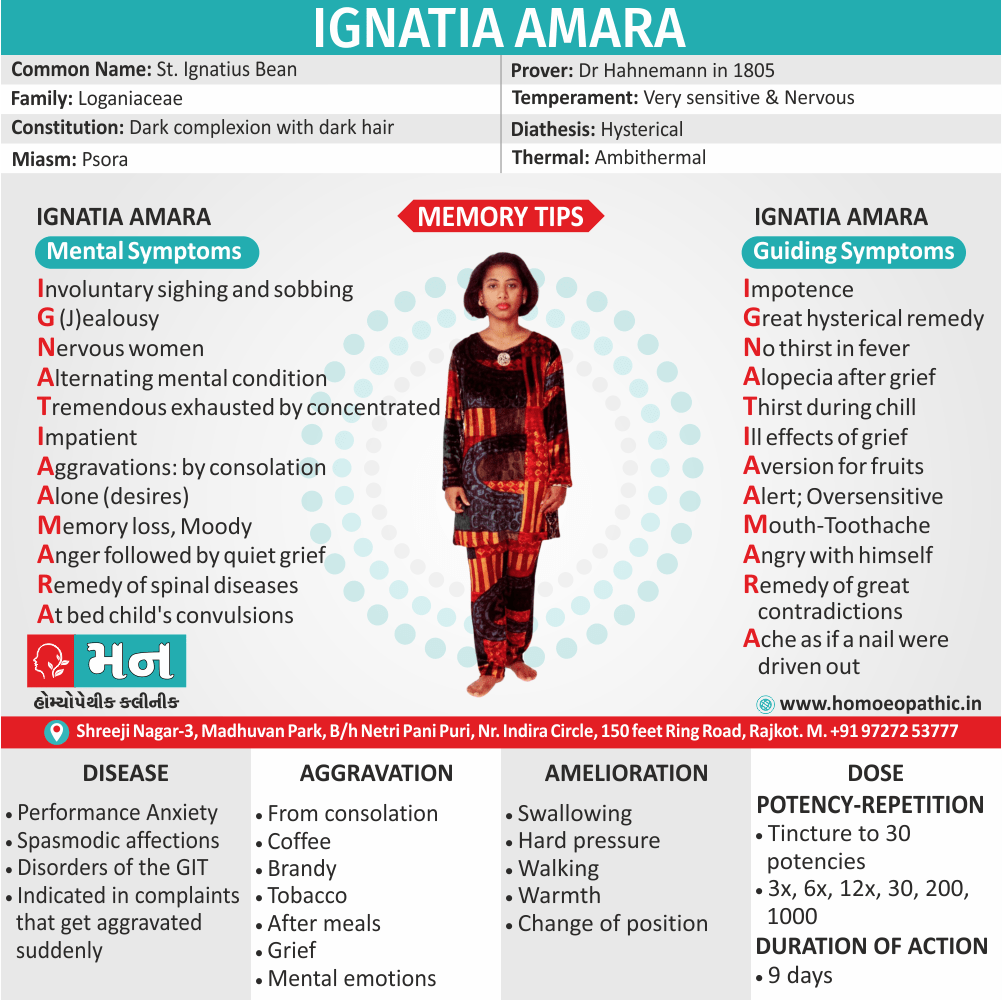
Ignatia
- Feeling of lump that cannot be swallowed.
- Swallowing difficult on account of inflamed, swollen and ulcerated tonsils.
- Tendency to choke, globus hystericus. Sore throat.
- Stitches when not swallowing.
- Worse – morning, after meals, liquids, grief. Better – eating something solid.
Kali carb
- Especially indicated in Sticking pain as from fish bone.
- Moreover, Swallowing difficult, food goes down esophagus slowly.
- Worse – soup also coffee.
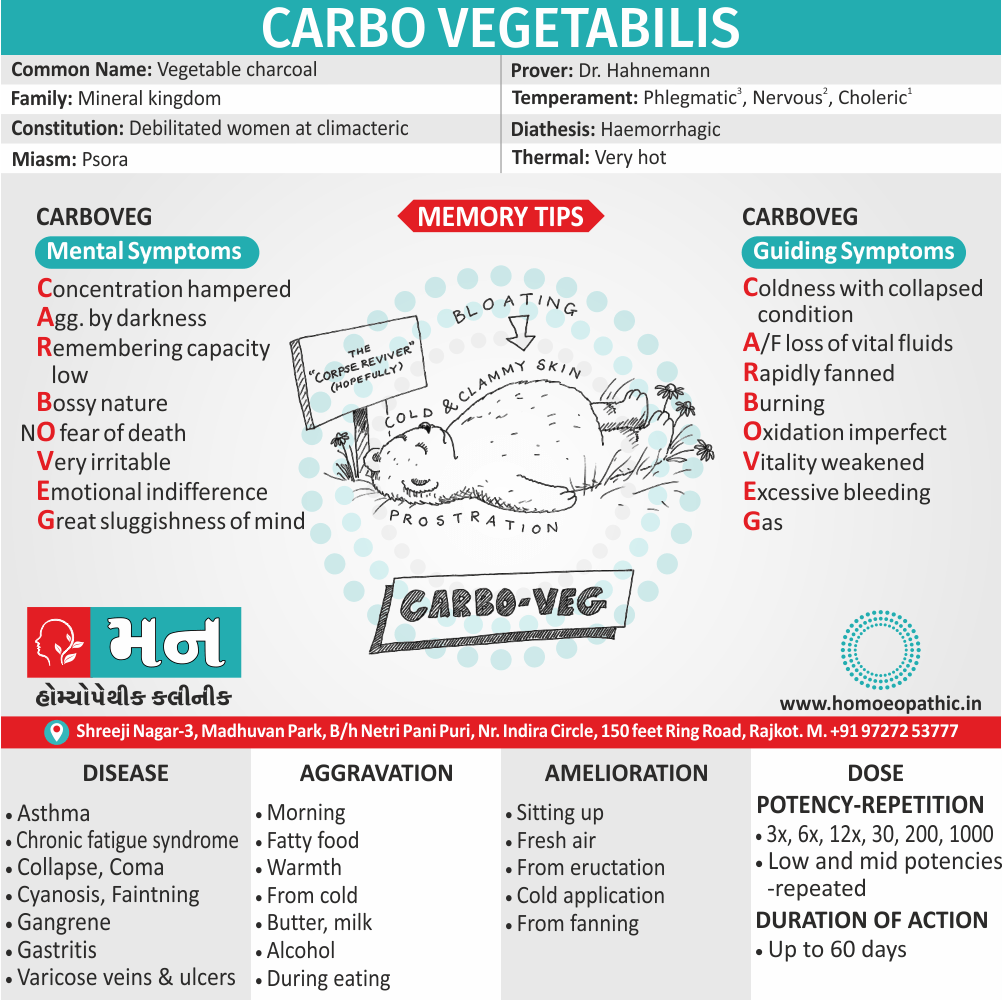
Phosphorus
- Generally, Burning in esophagus.
- Stricture of esophagus. additionally, Dryness in pharynx.
- Furthermore, Thirst for very cold weather. Cardiac opening to stomach seems contracted, too narrow.
- Vomiting throws up ingesta by mouthfuls.
- Worse – touch, warm food or drink. on other words, Better – cold food.
Silicea
- Stinging pain on swallowing.
- Besides this, Periodical quinsy – causing difficulty in swallowing.
- Pricking as if pin in tonsil.
- Worse – especially in morning, lying down.[1]
Diet and Regiment
- Avoiding acidic or spicy foods, mouthwash or drinks containing alcohol, and tobacco smoking.
- Eating soft, creamy, and mild foods, such as cheeses, mashed potatoes, and yogurt.
- Avoiding rough and hard foods, such as chips, nuts, and some fruits and vegetables.
- Rinsing mouth or gargling (do not swallow) with a mixture of water, salt, and baking soda.
- Eating and drinking lukewarm or cold foods and drinks; frozen fruit or ice pops may be soothing.
- Eating sour cream before each meal to coat the mucous membranes.
- Staying hydrated by drinking small amounts of liquids throughout the day.
- Reducing risk for GERD by maintaining a healthy weight and avoiding irritating, acidic foods, including tomato-based foods, citrus, and chocolates.
- Avoiding eating large, fatty meals right before bed.[2]
Frequently Asked Questions
What is Dysphagia?
Dysphagia difficulty with swallowing refers to problems with the transit of food or liquid from the mouth to the hypopharynx or through the esophagus.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Dysphagia?
- Arsenicum Album
- Alumina
- Baptisia
- Baryta carb
- Belladonna
- Cicuta
- Ignatia
- Kali carb
- Phosphorus
What causes Dysphagia?
- Achalasia
- Diffuse spasm
- Esophageal stricture
- Esophageal tumors
- Foreign bodies
- Esophageal ring
- GERD
- Neurological disorders
- Pharyngoesophageal diverticulum
What are the symptoms of Dysphagia?
- Pain while swallowing
- Inability to swallow
- Drooling
- Hoarseness
- Food coming back up (regurgitation)
- Frequent heartburn
- Food or stomach acid backing up into the throat
Reference used for Article Dysphagia
[1] Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies
[2] https://www.medicalnewstoday.com/articles/320621
[3] Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
[4] https://www.mayoclinic.org/diseases-conditions/dysphagia/symptoms-causes/syc-20372028
[5] https://www.mayoclinic.org/diseases-conditions/dysphagia/symptoms-causes/syc-20372028
[6]Dysphagia physical examination – wikidoc